
Caregiver blogger, Melissa Johnson, shares 31 tips and strategies she uses to help her husband cope with his TBI in a more effective manner.
1. Use a Mobile Calendar App
I created a calendar for Sean in my iPhone and shared it with him (see brief instructions below or click here). Now I can add his appointments, meetings, and trips on my phone and he is able to access them through the app on his iPhone and iPad. In addition to time and date, I can add the location or notes for the event. The app allows me set alerts which come across both our mobile devices as notifications. I normally set alerts a day in advance and an hour in advance to allow me time to remind him and avoid last-minute surprise. Using the calendar also helps me track his events that aren’t on my personal schedule (such as VFW meetings). I check the calendar each night and remind Sean of the next day’s schedule. It’s handy because i can manage it for him, see any items he adds himself, and view my own calendar at the same time.
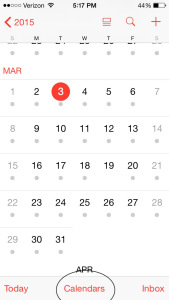
Open the iPhone’s calendar app and click on “Calendars”:
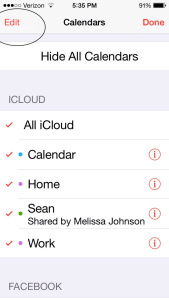
Select “Edit” under iCloud Calendars:
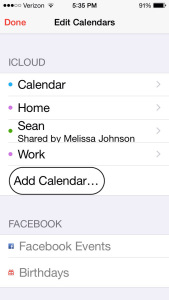
Select “Add Calendar” and follow instructions for naming calendar:
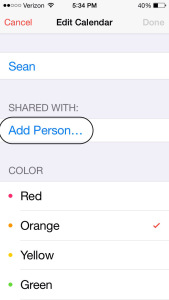
Select “Add Person” to share the calendar:
2. Sign up for Cozi
Visit cozi.com and sign up for their shared online calendar (I use the free version). Cozi offers shared calendars and lists that can be accessed by any family members with login information on their computers or mobile devices. You can opt to text individual mobile devices with appointments and notes automatically. I use Cozi to send Sean text messages each day reminding him to take medications and when to eat meals. I have the texts sent to my phone as well so I can verbally remind him (in case I lose track of time). There is room to add notes to each event, so messages sent can be as detailed as needed.
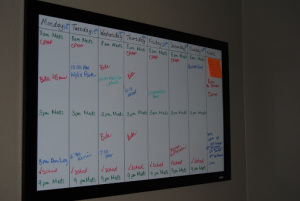
3. Develop a White Board Schedule
We started with a very detailed daily schedule to help Sean remember the progression of each day’s tasks. It worked well for a time, then reached a point where it overwhelmed him visually and cognitively. We now use a simpler version and combine it with text reminders for medications, meals etc. and verbal reminders.

4. Hold Daily Meetings
Choose a time of day that is structured (not over dinner, while doing homework with the kids, or while distracted with other activities) and is a typically a good time of day for focus. Sean and I chose to have our meetings each morning. This time was set aside to review the day’s activities, discuss needs, and address any military or VA issues or answer questions he had (to avoid fixating on these issues all day long—which had become a huge problem). We recorded a few notes in a notebook so he could look back at the discussion if he had questions later in the day, or needed a reminder of what we decided. Gradually, we have moved away from structured meetings since we don’t deal with the same volume of VA and military issues at the moment, and instead do a brief check in each morning to cover his schedule. I also check the calendar on Sunday night and alert him to upcoming activities and appointments for the week ahead.
5. Use a Timer
Time can be difficult to track for a person with a TBI. Setting a timer can help add structure to the day, aid in staying on task, and improve efficiency and independence. Try setting a timer to:
- Break tasks into smaller steps
- Allow for scheduled breaks
- Set start or end times for activities
- Allow transition time
6. Use Labels
TBI can make it difficult to remember where items are stored, and looking through multiple cupboards and drawers can add frustration. We use a system of labels around the house to locate key items. After our home remodel a couple years ago, Sean found the increased number of light switches especially confusing, so I labeled those as well. You may want to label drawers, cupboard doors, bathroom cabinets, nightstand drawers, storage in the garage, etc. to fit the needs in your home.

It can also be confusing, and even frightening, to operate appliances or equipment. Sean struggled for months to operate the new microwave since the buttons were different. Our new flat-top stove was a particular concern as the burners have options for different sized pans, and the surface stays hot long after the burner is turned off. I printed brief instructions for each appliance, mounted on a magnetic sheet, and covered with laminating film so they can be wiped clean, if needed. We also used orange bump dots to mark the buttons he may need to use most to make them more visible.


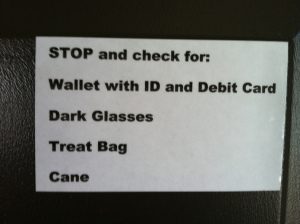
It’s easy to forget the items you need when you leave the house. I hang notes on doors (try colored Post It notes), and set necessary items on a chair next to the back door where they will be visible on the way out. I also made magnetic notes for items Sean needs each time he leaves the house.
7. Keep Things in the Same Location
When our daughter was home last summer she helped put groceries away and moved the yogurt to the opposite side of the refrigerator shelf. Sean thought we were out of yogurt for days when in fact we had plenty–just in the wrong spot. The same happens if I wash a bag of carrots and put them in a Tupperware bowl to preserve freshness. I now label that container so he knows what’s inside (the same for fresh cut fruit or vegetables) with reusable wipe-off labels.
Staying organized is a matter of establishing a habit for most of us. Many times I can’t find my wallet, keys, or phone if I put them in new locations. We have a shelf by the door for Sean’s keys and wallet. His medications for the day go on the same counter each morning. His chargers stay plugged in next to his nightstand. His hearing aids stay on top of the dresser. He has a small set of stacking drawers on his dresser for extra keys, cords, and eyeglasses. This routine aids with memory when he can’t locate an item.
8. Simplify Household Chores
Keep chores simple. We have learned that multi-step instructions or long lists of tasks overwhelm Sean’s brain and result in nothing being accomplished. To enable him to be helpful and avoid nagging we’ve come up with our own system.
Sean has a few tasks that he is in charge of completing. I can remind him with a note on the counter, but then allow plenty of time for him to complete the job independently. He is in charge of taking out the trash, feeding the dogs in the afternoon, keeping his area in the basement clean and organized, and putting away leftovers after each meal. In order to ensure he is completing chores independently, I do not step in to take over or redo what he has done. This means the trash might sit in the porch for a couple days until he remembers to pick it up and take it outside (though I remind him more frequently if it has food waste or it’s hot outside).
Sean still enjoys maintaining our home and yard, although he’s not able to do many tasks independently. He is no longer able to safely mow the lawn or shovel the snow. Since I have no desire to do either, our solution was to locate dependable people who offer those services and make it Sean’s job to call them when needed. At times it takes a day or two for him to remember to make the call, but the responsibility for doing so is solely his. He also calls to schedule car maintenance or home repair and I help him identify the person to call when necessary.
It’s important to note that changes in our routine (illness, pain, travel, company) will disrupt his routine and we will need to start over getting him back on track.
9. Create a Safe Space
Sensory overload and stress can lead to fatigue, anxiety, and anger. Having a safe space to retreat and decompress is an easy way to take time away and calm down or rest. Choose a quiet place that can be dedicated to relaxing activities. Equip this space with whatever you find comforting: TV, headphones, computer, comfortable chair, puzzles, books, etc. It is helpful to have items dedicated only to this space, with spares for other areas of the house, so this area is always prepared and ready.
When spending time at the home of relatives or friends, try to identify a safe space ahead of time. Talk to the host about the purpose of this space and ask them to help you select a location. Bring portable headphones, laptop, iPad, books, etc. in a back pack as a “mobile safe space.” Prepare ahead of time by discussing the plan and visit the safe area when you arrive.
Be aware of clues. For example, if Sean disappears with no notice I know he is taking down time and doesn’t need my support, but if he is seeking my attention, he needs me to direct him to the safe area and help him get settled in. He may need pain meds or extra support.
It may also be helpful to choose a safe word or code word that can be used during times of distress.
10. Using Tools to Aid Memory
Highlighters and Post-It notes or sticky tabs are great for marking important information in books, binders, and manuals. They are also handy if you print emails, memos, or meeting notes.
Digital recorders can be used to record meetings or classes, but can also be used to keep audio notes or reminders throughout the day. Most smart devices have digital recorders built in, so there is no need to purchase a separate device.
Lists can serve a variety of purposes. Sean is currently using a small whiteboard to track his to-do items for bike camp along with his weekly schedule. He keeps a Post-It note on the counter where he can jot down things he needs me to know (which can range from grocery items to appointments or tasks) and I can add to the calendar or to my own list. We also keep a list of his goals on the bulletin board along with a list of upcoming travel dates. The key is keeping all these lists in one location so he knows where to find them.
11. Track Health and Activity
It is important to document health changes and symptoms to identify patterns and track changes over time. Many times when doctors ask Sean how has been feeling, his answer is based on how he is feeling at the moment because he can’t recall how his mood or pain has been over the past few weeks or months since he last saw the doctor.
I make brief notes each day on Sean’s level and type of pain, if he uses additional medications, his sleep quality, nightmares, periods of confusion, etc. along with his activity levels such as riding his bike, walking his dog, or attending events and meetings. This enables us to give his providers the most accurate picture of his overall health and activity.
12. Manage Medications
Medication errors can be harmful or even fatal. Be sure to keep all medications in a safe place (we use a small safe) out of reach of children. Store medications in their original containers with pharmacy labels intact. Double check dates on labels for expiration and refill information.
Since Sean takes many daily pills, we use a pill sorter designed to hold a week’s worth of medication and divided into slots for AM, noon, and PM medications (the Velcro at the top of each box is to help him identify the AM container due to diminished vision). Occasionally, Sean gets confused and takes pills from the wrong slot at the wrong time of day, so we use a small jar with a lid to avoid confusion.
We keep an up-to-date printed list of medications in the safe, my purse, Sean’s wallet, and with emergency information.
If you receive prescriptions from the VA, you can use My HealtheVet to manage prescriptions and refills.
For more information, read this article about VA prescriptions from Family Of a Vet.
13. Find a Hobby
Keeping the mind and body active is an effective tool against depression, anxiety, and even pain. After an injury, it can be difficult to stay active and enjoy the same activities as before. Finding a hobby is one way to stay connected with others and constructively deal with stress and tension.
Exploring different hobbies can open your mind to new and creative endeavors. Engage local friends and family members to increase your amount of social interaction. Check your local area for hobby groups that have clubs or meetings. Take a class to learn something new.
Take time to explore alternatives and get connected with groups that offer adaptive sporting programs like Challenge Aspen Military Opportunities, Lakeshore Foundation’s Lima Foxtrot program, USABA, and Higher Ground (a few of many available to veterans). Building new skills is an excellent strategy for coping with changes in your life.
Volunteer activities can also offer a fantastic outlet and can become a hobby of sorts, too. The focus is on finding new activities to keep you active and healthy.
14. Allow More Time to Complete Activities
Cognitive deficits due to TBI can cause a variety of processing and attention difficulties. The following are key areas that can impact success when completing tasks and activities:
- Difficulty sustaining concentration for a period of time
- Inability to filter or combine information
- Losing track of time
- Fixating on one aspect of the task, unable to move forward
- Inability to make decisions, or making quick decisions which are not thought out
- Memory and confusion issues
- Slower processing time
It is important to allow time to think and respond, and provide prompting as necessary. Good ways to assist include:
- Be generous with wait time.
- Limit the number of steps.
- Use note cards or prompts.
- Remember building toward independence is a process.
15. Use Photo Albums to Aid in Memory
Several years ago Sean and my dad went on a fly fishing trip to Sun Valley Idaho. A few weeks later a friend asked Sean about the trip. Sean gave a blank stare and said he hadn’t been on a fishing trip. Several other times Sean has had difficulty remembering the events of trips, and the people he has met. I have put together small albums from each trip to help Sean recall these events. I have used labels to help him identify people. We look at the photos together and talk about what he did that he enjoyed. Slowly, people he has met multiple times have stuck in his memory. It’s handy when he asks questions about a trip, or about someone he’s met, to have the photos close at hand.
16. Use a Script
That might sound funny at first, but it’s incredibly helpful. I have found over the years that having scripts for the children when they are assisting Sean can make for a much smoother visit. I have included a few examples. Be sure to make note of what works in your individual situation.
Our daughter was staying with Sean and he was requesting to eat out every night. She had purchased groceries and was getting frustrated with his wanting to change her plans every night. I explained that he was probably getting hungry and making suggestions simply as a way to solve his hunger problem. I told her that as it neared dinner time she should tell him, “I’m making ____ for dinner tonight. It will be ready around 6:00.” The simple act of making him aware of what was coming next was enough to put him at ease.
When he gets anxious in public we practice using calming words such as, “We will be finished shortly.” “I understand your frustration, let’s finish up and get out of here.” “If you need to leave, just let me know.” Hearing the phrases he is used to helps him remain calm, and helps whoever is assisting him know what to do in tense situations.
When Sean is having a migraine the pain is normally compounded by confusion. He repeatedly gets out of bed, or asks what he should be doing. It is helpful to say, “You need to lay down (take a pill, use an ice pack, stay still) until you are feeling better. That’s your only job right now.” I may need to repeat it a few times, but it works much more effectively than trying to answer each question or concern he raises.
17. Manage Stress
Stress is a normal physical response to events that make you feel threatened or upset your balance in some way. Stress can also impair cognition, processing, and memory, and prolonged stress can wreak havoc on the entire body. It’s important to take time to restore the balance in your body and brain on a regular basis. Here are a few ways you can recover from and reduce the stress in your life.
- Get regular exercise.
- Eat a healthy diet.
- Practice good sleep habits.
- Reduce caffeine and sugar intake.
- Avoid alcohol, cigarettes, and other drugs.
- Take regular breaks.
- Learn to say no.
- Take time to connect with others.
- Find activities that replenish your soul.
18. Stick to a Routine
Individuals with brain injury may have difficulty planning and organizing their daily tasks. It is helpful to plan out a consistent routine at home that is predictable. Get up at the same time each day. Perform hygiene tasks in the same order. Eat scheduled meals. Use checklists where necessary to help stay on track. Predictability can reduce anxiety about the unknown and consistency will increase the level of independence in the home.
19. Travel Wisely
Travel can be stressful even under the best of circumstances. Being prepared can ensure your travel plans go as smoothly as possible.
Use a specific packing list. Sean often means to pack an item, or thinks he has it when he doesn’t. Having a list to check off allows him to pack independently and be confident he has all he needs.
Bring enough medications (prescription and over-the-counter as needed). Include an extra day or two to allow a buffer should travel plans change. Be sure to include extra pain medications. Always keep medications and any critical care items in your carry-on baggage should flights be canceled or delayed
Pack a variety of comfort items and activities such as a travel pillow and blanket, books or audio books, portable electronic device loaded with music or games, headphones, and snacks. Sean packs the items he needs in his backpack whether we are flying or driving so he has them close at hand.
If you have a service dog, be sure to include treats and comfort items along with necessary care tools and plenty of food. Keep the dog’s critical items in your carry-on baggage. It’s helpful to have ADA guidelines available along with service animal guidelines from the Air Carrier Access Act (see Seat Assignments page 6) should you encounter any questions or concerns about your service animal.
If driving, be prepared to make stops along the way and allow break time.
When flying, allow enough time to comfortably get through security and to gates on time. TSA offers a service for disabled veterans that will provide assistance at the airport. Contact the TSA Cares Helpline for more information.
When you arrive at your destination, allow time to settle in before starting activities.
If you are staying in a hotel, locate nearby restaurants or choose a hotel with a restaurant onsite. Dine at off-peak hours to avoid crowds.
If using public transportation, study the routes and fares ahead of time. Have taxi fare and reliable cab company numbers on hand. If driving, know the best routes around town and the locations of your destinations.
Have a clear (but flexible) itinerary with planned breaks and meal times.
Remember that when you return home extra recovery time will be needed before starting your normal routine.
20. Prepare Simple Meals
One of Sean’s goals is to help plan and prepare meals a couple times a week. Sean received training in safe cooking techniques during his blind rehab programs and is interested in becoming more independent in the kitchen.
- Plan the menu and shopping list. Choose meals with fewer steps to follow.
- Store all items in one spot with a label in the cupboard and/or refrigerator.
- Use a tray to gather ingredients at preparation time. Gather needed cooking utensils in the same fashion. Have a timer available.
- Use recipe cards with clear steps. Follow all steps in order and use the timer to signal when it’s time for the next step.
- Practice kitchen safety.
- Include clean up as part of meal prep.
You might also try make-ahead freezer meals that can be reheated by following instructions taped to the container. Convenience meals such as microwave meals, frozen dinners, or sandwiches are another easy way to share in the cooking responsibilities.
21. Prepare for Absence or Illness
Preparing to be away from home (or, gasp! sick) can be incredibly stressful. By planning ahead of time (when possible) you can make your absence easier for all parties. Pre-planning is especially valuable when absences come as a surprise.
Identify how the care recipient will:
- get to and from appointments, meetings, and outings
- get meals or groceries (and/or remember to prepare and eat meals)
- stock up on microwaveable meals, canned goods, frozen foods, juices
- remember to take medications
- care for pets
- stay on a sleep schedule
- clean up
Identify people who can assist with daily tasks, or who can stop by during the day to check in.
Have a list of emergency number on hand.
Have copies of medication lists, doctors, insurance information in a central location.
Help your loved one identify what he/she can do to help you. Being helpful and providing care for you is an easy way to put anxieties to rest.
22. Emergency Information
Always carry emergency information in your wallet or purse. This information should include medical conditions, doctors’ information, current medications, and insurance information along with any emergency contact numbers.
As an added measure, you might consider a free AVBI Medical Alert Tag and ID Card through American Veterans with Brain Injuries.
A new option available for purchase is My ID band which allows medical professionals to electronically access your emergency information.
Smart phone users can download an app such as ICE (In Case of Emergency) which displays emergency information on the lock screen in case you are in an accident.
23. Create an Emergency Binder
I know what to do in an emergency involving Sean. I carry his critical medical information and know his history. But what if an accident occurred and I was not the person on the scene? What if something happened to me, would he know what to do? Creating an Emergency Binder could literally save a life.
Things to include:
- Personal Information (for each family member): name, SSN, DOB, height, weight
- Copies of insurance cards, VA ID card, military ID
- Allergy information
- Names of doctors with specialties and contact information
- Brief medical history, including any mental health conditions
- Current medications and dosages with prescriber and pharmacy information
- Emergency contact numbers for family members
- Copies of legal documents such as a Durable Power of Attorney for Health Care, Living Will, and Advance Directives
If you are interested in a free, ready-made packet you can print and fill in, email me at melissa@familyofavet.com and I will send to you.
Also, be sure to post emergency numbers in a visible location and include suicide hotline numbers.
24. Use Apps
Check out these Life-Changing Mobile Apps for People with Brain Injury.
From this list Sean uses Audible, Cozi, ICE, Lumosity, PTSD Coach, Dragon Dictation, Breathe2Relax, and T2 Mood Tracker. Check them out and see what might work for your situation.
Sean also uses Brain Fit and Brain Trainer apps occasionally. He has the MyLocation app which allows a user to find their location and share with others. Sean’s is set up to send me his location if he is confused or lost.
25. Educate Family and Friends
It can be incredibly difficult for family members and friends to understand the changes that happen after injury. This is especially true when dealing with an invisible injury like TBI. It’s important to have a support system that includes loved ones, which means you may need to take an active role as educator to help them understand how the injury has impacted the immediate family, as well as the care recipient, and how they can best be of assistance.
Be prepared to have difficult conversations. Whether discussing care concerns or expressing a need for space and privacy, conversations with family members can be touchy post injury.
Have realistic expectations. Every member of the team has different abilities, skills, comfort levels, and limitations.
Be clear about who is in charge of making care decisions, and what medical information will be shared.
Share strategies that work. Encourage others to get involved in positive ways by following the model that works for you.
Make necessary adaptations for holidays and events. Discuss strategies for success in advance.
Most importantly, be sure all members are educated about the nature of the disability and expected outcomes. Share information on TBI that you find helpful. You can find tons of helpful articles and videos at Brainline, Brainline Military, and Family Of a Vet. Also check out Brain Injury Association of America and American Veterans with Brain Injuries. Visit your local county extension office, or do a quick google search, for local brain injury agencies or support groups.
26. Keep a Journal
Journaling has been shown to help reduce symptoms of anxiety and depression and improve overall feelings of self-worth. Taking time each day to jot down notes about the events of the day and how you felt throughout the day is an excellent tool to help get in touch with emotions and process feelings. By reading through previous journal entries you can identify common stressors or triggers and develop a plan for positive coping strategies when those triggers arise. Depending on your preference, a personal journal can be shared with doctors or counselors for more insight.
For those with TBI, a journal can also serve as a reference book to record events and memories. It’s easy to look back and see when something happened, or browse through entries to refresh your memory.
If paper and pencil isn’t your thing, or you’re on the go, try using a digital voice recorder to dictate your journal entries
27. Keep it Simple
Eliminate what you can. Think you can’t? Start by reviewing activities for each family member. Evaluate your choices. Why are you involved with each activity? Is this activity meaningful and necessary? Does this activity enrich our lives in long-term ways? If not, consider eliminating it. Keep in mind that the goal is to streamline your home life and relieve stress and tension from your family.
Consider your options. You won’t be the world’s worst parent if you don’t attend every single game. Talk to other parents about carpooling to activities. There are usually other parents who would be relieved by a rotating schedule. If a season-long program doesn’t fit into your schedule, check into local day camps or classes your child could attend. Choose activities where your child is adequately supervised and time is structured to gain time for yourself. Use this time to run errands, or, bring a good book and enjoy a little down time.
Don’t do things simply because you’re feeling pressured. While it may be easier to say “yes” in the moment, think about how you will feel once you are obligated. If it’s not the right choice for you say “no” and stick to it.
What can you outsource? Do you have a neighbor who can share carpooling duties to and from school? Is there a friend or family member who can take the kids off-site for playdates? Can you afford to have someone come in to clean or have groceries delivered? Check with your local VA facilities, veterans’ organizations, or churches for additional resources and services.
Be honest about your needs and limitations. Many times people want to help but don’t know how.
Utilize available services such as Occupational Therapy, Speech Therapy, Physical Therapy, or Recreation Therapy along with services through any available caregiver programs. These trained professionals have a wealth of information and resources.
Forgive yourself. No one is prepared for major life changes. It’s ok to not have all the answers or to not have your sh*t together all the time. We all struggle to get through the day at times and find it takes much longer to recover after setbacks or when new issues arise.
28. Get Plenty of Sleep
Sleep is essential to good physical and mental health. When you don’t get enough sleep memory, concentration, coordination, and mood are negatively impacted. Lack of sleep over a period of time causes your physical health to decline and can lead to increased depression and anxiety. Sean’s nightmares, night sweats, insomnia, fatigue, restless leg syndrome, sleep apnea, and chronic pain all have a negative impact on his quality and quantity of sleep (and mine!). Sleep medications help with some of the symptoms, but don’t solve the problem.
To combat sleep deprivation and allow your body as much rest as possible, establish a sleep schedule by going to be and waking at set times each day. Take naps, if needed, early in the day. Avoid if napping disrupts nighttime sleep.
Turn off electronics. Keep the room dark and cool. Make the bedroom a quiet space, or use a white noise machine to create an audibly peaceful environment. Invest in a comfortable mattress, pillows, and bedding.
Avoid caffeine and sugar after dinner, and don’t eat large meals late in the day. Alcohol and nicotine can also be factors in quality of sleep.
Take time to unwind before bedtime. Read, meditate, or practice deep breathing exercises. Take a warm bath. Listen to soothing music. Dim the lights. This can help your body and brain get into sleep mode.
29. Encourage Independence
Independence is a critical component of recovery after TBI. While your loved one may not be able to do all their former activities to the same extent as before the injury, implementing support and modifications can maximize independence.
- Set realistic goals and start small.
- Create an environment for success. Have needed materials on hand in areas where they are easy to access.
- Use checklists or verbal prompts where possible.
- Practice safety and good judgement.
- Give immediate, constructive feedback. Use praise and encouragement.
- Accept that mistakes will happen and make modifications when necessary.
- Connect with others who will encourage independence in or out of the home.
30. Use Praise and Positive Affirmations
A little praise can go a long way toward boosting a person’s mood and creating a positive pattern of behavior and interaction.
- Remember to say, “Thank you.” Even for the small things like taking out the trash (even if it takes several days to get it done) or wiping off the table.
- Leave little notes of appreciation around the house.
- Share your pride in their accomplishments.
- Keep a gratitude journal.
31. Resources
Looking for additional information on traumatic brain injury? Check out these websites:
- Brainline
- Family Of a Vet
- Department of Veterans Affairs
- Defense and Veterans Brain Injury Center
- American Veterans with Brain Injury
- Brain Injury Association of America
Additional resources and reading material available on tabs at the top of this page.
About the Author
 Melissa Johnson and her husband, Sean, were married in 1995 and raised their three children in Aberdeen, SD. Melissa taught for 15 years in Special Education and First Grade. Sean served in the US Army and was deployed three times in his 24-year career in the military. Sean was injured by a mortar blast on March 25, 2006, in Balad, Iraq. The blast resulted in a traumatic brain injury. Sean is also legally blind and struggles with post-traumatic stress disorder.
Melissa Johnson and her husband, Sean, were married in 1995 and raised their three children in Aberdeen, SD. Melissa taught for 15 years in Special Education and First Grade. Sean served in the US Army and was deployed three times in his 24-year career in the military. Sean was injured by a mortar blast on March 25, 2006, in Balad, Iraq. The blast resulted in a traumatic brain injury. Sean is also legally blind and struggles with post-traumatic stress disorder.
When Sean returned home in 2007, the family struggled to adjust to this “new” man in their house. Melissa eventually left her teaching job to become a full-time caregiver to her husband. She is now a certified caregiver through the VA’s Caregiver Program.
Both Melissa and Sean have been active with the Blinded Veterans Association since 2009. Sean serves as Commander of his local VFW chapter and is also the Junior Vice of the local Disabled American Veterans chapter. Melissa currently works with the Military and Veteran Caregiver Network as the Education and Training Coordinator. She serves with the Elizabeth Dole Foundation as a Caregiver Fellow. She is honored to work alongside other caregivers from across the nation to raise awareness of the issues facing our nation’s caregivers and families.
Read more from Melissa on her blog: Bringing the Battle Home

Comments (24)
Please remember, we are not able to give medical or legal advice. If you have medical concerns, please consult your doctor. All posted comments are the views and opinions of the poster only.
Anonymous replied on Permalink
I acquired my TBI in 08 and have been through all the recovery to get back to my feet with out any assistive device. I also did some volunteering for about 4 years. Blessed to find a job with the therapy pool I was using. Unfortunately the location became to much for the city to sponsor. With determination and grit I found another job with Costco. I’ve come to the point where I feel I can live more independently ( move to my own place). I would appreciate assistance on the steps involved from those willing to help.
Thanks
Anonymous replied on Permalink
Thank you so much for sharing. This is very helpful. I recently came across a program that may help veterans and first responders that have had a brain injury. It is free and may help your husband or people like him. Thank you again for sharing. If interested, the website for the program I mentioned is: https://ufhealthjax.org/brain-wellness/
Rae Z. replied on Permalink
This is wonderful! Doctors should give this to their patients. I am going to use many of these!
Anonymous replied on Permalink
I have lived with a brain injury for 3 years now, and it is a nightmare.
Steve L replied on Permalink
8 so far. Agree. I was about to finish bachelors and teach kids. Had to quit totally. Now can't drive and agree. Is a nightmare.
Feller replied on Permalink
This is a GREAT article, and after my brain injury, my phone calendar and reminders are so critical, not to mention GPS! Its helped me stay semi independent, and still driving even though they said I would when I was discharged from the hospital.
Anonymous replied on Permalink
extraordinary people, that show us the path.
Patti Talley replied on Permalink
Thank you. I have been trying to read up on this. My husband is coming home this week. I have just been. So worried on how I am going to take care of him. You have been very..insightful.
Anonymous replied on Permalink
Thank you for sharing this excellent artice and for sharing your story...
Anonymous replied on Permalink
I'm a professional organizer and have a new client with TBI. I found this list extensive and very helpful. You are Ah. Mazing!
Anonymous replied on Permalink
Does anyone know if it is normal to take 1 hour naps about twice a day in the afternoon. It does not seem to interfere with his nighttime sleep. My husband had a TBI in February he gets headaches almost everyday they are not bad but he said they annoy him.after he naps his head feels better .
Kelly Worthen replied on Permalink
I found this essential for my own recovery when the “wall” of fatigue and headaches hit. I too, would feel so much relief afterwards.
BrianC replied on Permalink
Hello. Yes, it is normal when having TBI to have a few naps during the day,,somedays,,not twice but the feeling of being tired is normal. and as for his headaches,,He might be suffering from Occipital Nuroalgia, I have TBI and havehad an injury to my occipital nerve, and that caused my headaches huge, the occipital nerve at the base of his skull is what causes headaches. CBD oil has made a huge difference in slowing down my headaches so..might be worth a try,,good luck..
wENDY replied on Permalink
YES VERY NORMAL AND GOOD. I WAS TOLD TO TAKE A NAP AT THE SAME TIME EVERY DAY TO ALLOW THE BRAIN TO HEAL MORE QUICKLY.
O.M replied on Permalink
Thank you
jams replied on Permalink
thank you so much for sharing. wonderfully amazing advice and helpful to anyone with an injured or recovering brain. alas brain injuries are not always visible and thus life can be a bit more of a struggle. maybe if the more people understand any form of brain injury, the happier life will be:)
Norah replied on Permalink
Thank you for this checklist! My husband is a veteran. His TBI came from a car accident. Your checklist is a great thing to have for him and me. We will use it daily!
Luke replied on Permalink
Thank you
Jenna H. replied on Permalink
Thank you, Melissa. My TBI happened 33 years ago when I was 13. Head injuries were not understood nearly as well then, especially in children. At 46 years old, I finally have a Psychiatrist that is treating me as a person with TBI instead of a person with various psychiatric disorders such as Bipolar or Generalized Anxiety. After just 2 months of recognizing the head injury as a primary cause of my difficulties, I am finally seeing some positive results and feeling some amount of hope for a better functioning future. Although I suspected the cause, I'm just beginning to truly understand why I have such a hard time accomplishing the most basic, daily goals. It helps to see how you and Sean have found ways to maneuver through day to day living.
Lisa replied on Permalink
Melissa, thank you for publicizing and sharing this information, it is extremely valuable.
Anonymous replied on Permalink
Lol. This makes me feel good! I've been living with my tbi now for the past 17 years. No one told me about this stuff. This is how I coped with life (minus the phone apps cause I wrote notes everywhere). I still struggle with things and yes, I do use my phone for a lot of reminders.
Anonymous replied on Permalink
Strategy no 32 - the most important one. Have a wonderful person like Melissa to help you with all this. Hats off to you Melissa for everything you do, and Sean, I know how hard it is.
Brandon replied on Permalink
I'm 14 year old go hit by a baseball the summer of 2018 and now I'm a TBI. I was searching this up because no one at school understands anything bout it and I get regected alot and hit In the head alot too. Thank you for making my life more understandable. Also, Sean thank you for your service. For Canada, Brandon Shearing
Elizabeth replied on Permalink
Good for you buddy!!! I can totally tell you that you are amazing!!! Promise me you will never stop believing in Yourself! You have got this!