Women represent the fastest-growing segment of the veteran population – they make up 9% of the total veteran population in the U.S. (U.S. Census Bureau, 2019), and are projected to make up 16% of all living veterans by 2043 (National Center for Veteran Analysis and Statistics, 2017). Of warriors who completed the 2020 Wounded Warrior Project® (WWP) Annual Warrior Survey, 20% are women – a larger representation when compared to the general veteran population.
As the population of women veterans continues to grow, understanding their unique challenges and needs is critical. Prior research has shown that post-traumatic stress disorder (PTSD) risk is higher among individuals with co-occurring mental health conditions, those who experience combat or sexual assault, and women. (Irish et al., 2011; Sandweiss et al., 2011; U.S. Department of Veterans Affairs, 2021). In line with this prior research, PTSD continues to be one of the highest stated problems among WWP women warriors:
In the 2020 Annual Warrior Survey, 80% of women warriors reported living with PTSD.
One warrior described what it’s like to live with PTSD:
“When you live with PTSD, you’re very aware of your surroundings; attentive to everything. Even little things can spark an episode. Think of having your worst day, and multiply it by 10. But it’s every day, not just one day. It keeps happening, and there is no way to stop it.”
PTSD is a mental health condition that typically occurs after witnessing or experiencing a life-threatening event (American Psychiatric Association, 2021; U.S. Department of Veterans Affairs, 2021). PTSD can happen to anyone – about 7% to 8% of the general population will experience PTSD at some point in their lifetimes (Gradus, 2007). Exposure to traumas uniquely associated with war and combat contribute to the disproportionate impact of PTSD among the veteran population (Price & Stevens, 2018), particularly those who bravely stepped forward to protect our country after the events of September 11.
In the 2020 Annual Warrior Survey, warriors were asked a series of questions that determined the severity of PTSD symptoms they were currently experiencing at the time of the survey. The analysis reported in this paper focuses on survey responses from women warriors registered with WWP, who were experiencing moderate to severe PTSD symptoms.
To better understand the prevalence of PTSD among women warriors, and the experiences that contribute to it, WWP conducted a more in-depth analysis of 2020 Annual Warrior Survey data. This analysis highlights three major PTSD risk factors prevalent among women warriors: combat exposure, co-occurring mental health conditions, and military sexual trauma.
PTSD Risk Factor: Combat Experience
Combat experience is a stressor service members are exposed to, leading to the potential of facing traumatic events while in service (Parker, Igielnik, Barroso, & Cilluffo, 2019). Combat-related trauma like exposure to potentially life-threatening events or witnessing injury or death to a fellow service member increases the risk of having PTSD or other mental health conditions. Many symptoms of PTSD are delayed until well after combat exposure (Crocq & Crocq, 2000).
According to the 2020 Annual Warrior Survey, women warriors were deployed an average of 3 times, of whom 84% were deployed to a combat zone.
Among women warriors, those who deployed to a combat zone are 1.2 times as likely to experience moderate to severe PTSD compared to women warriors who did not deploy to a combat zone.
PTSD Risk Factor: Co-Occurring Mental Health Conditions
Co-occurring disorders arise when an individual is diagnosed with more than one health condition and/ or substance use disorder, creating an entwined problem (Psychology Today, 2019). PTSD often occurs with other psychiatric disorders, particularly depression. Individuals with co-occurring mental health conditions often experience more severe psychiatric symptoms, worsening disease or injury, and increased risk for chronic persistence over time (Armenta et al., 2019; Campbell et al., 2007).
Co-occurring mental health conditions are highly prevalent among women warriors, with 91% reporting more than one mental health condition.
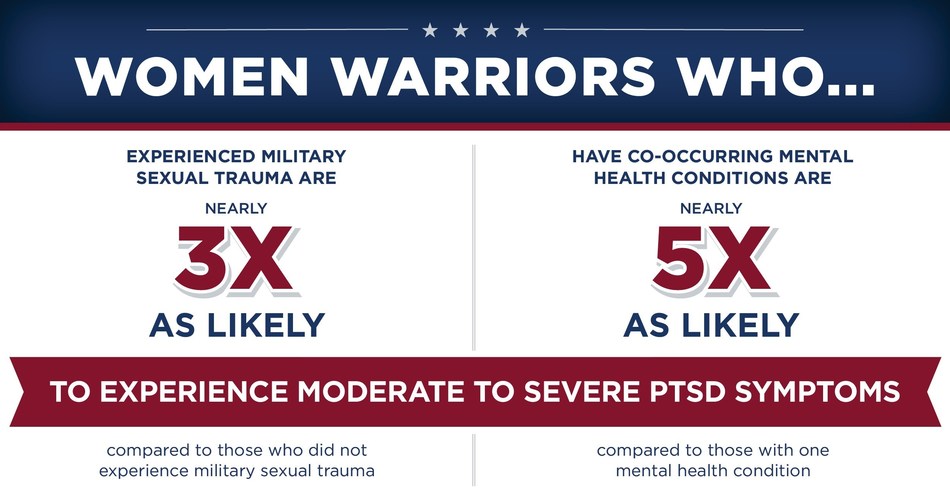
Women warriors with co-occurring mental health conditions were 4.7 times as likely to experience moderate to severe PTSD symptoms, compared to those with only one mental health condition.
Women Warriors with PTSD report experiencing an average of 4 mental health conditions. Along with PTSD, the most commonly reported mental health conditions among women warriors include:
- 84% Anxiety
- 81% Depression
- 81% Sleep Problems
PTSD Risk Factor: Military Sexual Trauma
Military sexual trauma (MST) is defined as sexual harassment or sexual assault experienced during military service. Among the general veteran population, women veterans indicate higher rates of MST compared to men; according to the Veteran Affairs (VA) health care’s national screening program, roughly 1 in 3 women and 1 in 50 men stated “yes” to experiencing MST when asked by their VA care providers (U.S Department of Veteran Affairs, 2020).
Similarly, among warriors registered with WWP, women are more likely to have experienced MST. In the 2020 Annual Warrior Survey:
11% of all warriors said they experienced MST, and of them, more than 3 in 4 (78%) were women (Wounded Warrior Project, 2020).
Women warriors who experienced MST were nearly 3 times as likely6 to experience moderate to severe PTSD symptoms, compared to women warriors who did not experience MST.
Access to Care
Given these challenges, access to mental health care is critical in ensuring that women warriors are empowered to live life on their own terms.
Nearly half of women warriors with PTSD had difficulty accessing mental health care.
Women warriors experiencing moderate to severe PTSD symptoms were nearly 3 times as likely to express difficulty getting mental health care, compared to women warriors without PTSD symptoms.
Top Three Barriers to Mental Health Care for Women Experiencing PTSD Symptoms:
- inconsistent or lapse in treatment
- felt treatment might bring up painful or traumatic memories
- difficulty in scheduling appointments
Supporting Women Warriors Living with PTSD
A combined approach – through both clinical and public health efforts – is essential for increasing awareness and availability of mental health care for women veterans. VA services combined with social and public health programs, like those provided by WWP, are vital to expanding access to care to support the short- and long-term physical and psychological well-being of women warriors.
WWP provides mental health and wellness programs that break down barriers to care and support warriors through each step in their journeys to recovery. From peer support to telephonic emotional support and intensive outpatient care, WWP helps warriors find the level of care they need.
Peer Support and Connection
WWP understands the critical nature of peer support in healing from combat-related trauma, co-occurring mental health conditions, and military sexual trauma. In fiscal year 2020 (FY20), WWP held more than 4,300 virtual and in-person connection events to keep warriors engaged with their peers and communities, and with the addition of virtual options, we saw an increase in participation from women warriors. Impact data show that these events – even when held virtually – are effective in building feelings of social support and meaningful connection.
After attending WWP Connection events, 91% of participants reported that they felt socially connected to their peers, and 89% said they feel that they have people they can depend on.
WWP also provides opportunities for women warriors to meet in small, warrior-led support groups where they can connect and bond over shared experiences in a safe, judgment-free environment. Peer support groups are an example of public health services that provide a safe space for veterans to connect and heal. Peer support groups provide a low-cost, widely available, and effective approach – that when combined with clinical care, can lead to better outcomes for positive coping, increased self-efficacy, and reduced clinical symptoms among veterans transitioning out of the military (Derebing et al., 2018).
Warrior Care Network
WWP partners with four world-renowned academic medical centers to form the Warrior Care Network®, to deliver mental health care during a 2-3-week intensive outpatient program that integrates evidence-based treatments with complementary alternative therapies. This unique veteran-centric approach increases access to treatment and improves outcomes for warriors living with PTSD, TBI, and related conditions.
In FY20, WWP provided more than 50,000 hours of PTSD treatment through Warrior Care Network. 76% of warriors who received this treatment experienced a reduction in PTSD symptoms.
With women experiencing MST at higher rates than men, Warrior Care Network offers an MST-focused intensive outpatient program, which treats cohorts of mostly women. During the three-week treatment program, participants build strong bonds with other veterans in their cohort who share similar trauma experiences.
WWP offers several mental health programs not listed here. To learn more about these, and our programs in other areas like physical and financial wellness, please visit woundedwarriorproject.org/programs.
WWP’s research helps shape the way we serve warriors, and brings greater awareness to the challenges they face in hopes that we, as a community, can support them throughout their journeys. We are committed to understanding the needs of women warriors as the female veteran population continues to grow, and we will continue to work tirelessly to break down barriers to care, connect women warriors with the resources they need, and advocate for them on Capitol Hill.
If you or a veteran you know is looking for mental health support, please do not hesitate to reach out to the WWP Resource Center by calling 888.WWP.ALUM (997.2586) or emailing resourcecenter@woundedwarriorproject.org.
Authors
Lara Berghammer, MPH
Lara Berghammer, MPH is a researcher for Wounded Warrior Project, where she supports the Annual Warrior Survey design and analytics. Lara first joined WWP in 2018, conducting program evaluation for physical health and wellness programs. Lara holds a B.S. in Biomedical Science from Texas A&M University and a Master of Public Health in Epidemiology from the University of Louisiana Health Sciences Center. She is currently a member and active participant with the American Public Health Association.
Amanda Peterson
Amanda Peterson is a senior researcher for Wounded Warrior Project, where she manages the Annual Warrior Survey and leads and contributes to internal and collaborative research initiatives that measure the impact and outcomes of WWP programs. Amanda first joined WWP in 2015, conducting program evaluation on WWP mental health programs. She holds an M.A. in Sociology from Middle Tennessee State University and undergraduate degrees in English and Sociology from the University of North Florida. Amanda is active in the research community and currently serves on the board of the Southeast Evaluation Association.
References
- American Psychiatric Association. (2021). What Is PTSD? Retrieved May 5, 2021, from https://www.psychiatry.org/patients-familiesptsd/what-is-ptsd
- Armenta, R. F., Walter, K. H., Rose Geronimo-Hara, T., Porter, B., Stander, V. A., & Leardmann, C. A. (2019). Longitudinal trajectories of comorbid PTSD and depression symptoms among U.S. service members and veterans. BMC Psychiatry, 19, 396. https://doi. org/10.1186/s12888-019-2375-1
- Campbell, D. G., Felker, B. L., Liu, C.-F., Yano, E. M., Kirchner, J. E., Chan, D., … Chaney, E. F. (2007). Prevalence of Depression-PTSD Comorbidity: Implications for Clinical Practice Guidelines and Primary Care based Interventions. Society of General Internal Medicine, 22, 711–718. https://doi.org/10.1007/s11606006-0101-4
- Crocq, M.-A., & Crocq, L. (2000). From shell shock and war neurosis to posttraumatic stress disorder: a history of psychotraumatology Dialogues in Clinical Neuroscience, 2(1). Retrieved from https://wwwncbi.nlm.nih.gov/pmc/articlesPMC3181586/pdfDialoguesClin Neurosci-2-47.pdf
- Gradus, J. (2007). Epidemiology of PTSD. Retrieved from https://www.ptsd.va.gov/professional/treat/essentials/epidemiology.asp#two
- Irish, L. A., Fischer, B., Fallon, W., Spoonster, E., Sledjeski, E. M., & Delahanty, D. L. (2011). Gender Differences in PTSD Symptoms: An Exploration of Peritraumatic Mechanisms. J Anxiety Disord, 25(2), 209–216 https://doi.org/10.1016/j.janxdis.2010.09.004
- National Center for Veteran Analysis and Statistics. (2017). Women Veterans Report: The Past, Present, and Future of Women Veterans. Washington, DC. Retrieved from https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
- Parker, K., Igielnik, R., Barroso, A., & Cilluffo, A. (2019). The American Veteran Experience and the Post 9/11 Generation. Pew Research Center. Retrieved from https://www.pewsocialtrends.org/2019/09/10the-american-veteran-experience-and-the-post-9-11- generation/
- Price, J. L., & Stevens, S. P. (2018). How Common is PTSD in Veterans? - PTSD: National Center for PTSD. Retrieved May 16, 2021, from https://www.ptsd.va.gov/understand/common/common_veterans.asp
- Psychology Today. (2019, February). Co-Occurring Disorders | Psychology Today. Retrieved May 16, 2021, from https://www. psychologytoday.com/us/conditions/co-occurring-disorders
- Sandweiss, D. A., Slymen, D. J., LeardMann, C. A., Smith, B., White, M. R., Boyko, E. J., … Smith, T. C. (2011). Preinjury psychiatric status, injury severity, and postdeployment posttraumatic stress disorder. Archives of General Psychiatry, 68(5), 496–504. https://doi.org/ 10.1001/archgenpsychiatry.2011.44
- U.S. Census Bureau. (2019). Veteran Status. Retrieved May 4, 2021, from https://data.census.gov/cedsci/table?q=United States&t=Veterans&tid=ACSST1Y2019S2101&hidePreview=true
- U.S. Department of Veterans Affairs. (2021). PTSD: National Center for PTSD Home. Retrieved May 5, 2021, from https://www.ptsd.va.gov/
- U.S Department of Veteran Affairs. (2020). What is military sexual trauma (MST)? How can MST affect Veterans? Retrieved from www.va.gov
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2018). PTSD Checklist for DSM-5 (PCL-5) - Standard [measurement instrument]. Retrieved from https://www.ptsd.va.gov/professional/ Wounded Warrior Project. (2020).
- 2020 Wounded Warrior Project Annual Warrior Survey: Report of Findings
This report was written by Wounded Warrior Project® (WWP).
Download your own copy of the PDF here.