Hear what happens to one young girl who has a minor TBI while snowboarding ... and a serious car crash months before.
Produced by Noel Gunther, Ashley Gilleland, Victoria Tilney McDonough, and Brian King.
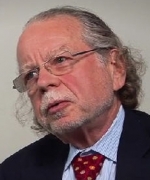
About the author: Wayne Gordon, PhD
Wayne Gordon, PhD, ABPP/Cn, is the Jack Nash Professor of Rehabilitation Medicine and associate director of the Department of Rehabilitation Medicine at the Mount Sinai School of Medicine. He is a neuropsychologist and the director of the Mount Sinai Brain Injury Research Center.