A combat medic in the wars in Iraq and Afghanistan encountered daily challenges years later as a Student-Veteran: “… I can’t remember anything unless I go over it a thousand times, I can’t keep focused on anything, and I just can’t seem to figure out a way to make myself better! I will be in lecture, and every time someone opens a door, stands up, coughs behind me too loud, or whatever, I go completely off the professor to look at what it is. Then I look back at the professor and I realize I’ve totally lost track of what they are saying, and as I scramble to catch up, I get so nervous about it, that I am again not paying attention to what he is saying!”
This is the lived experience of many Veterans who struggle with traumatic brain injury (TBI) and post-traumatic stress (PTS) symptoms. Difficulty holding information in mind, remaining focused in the presence of distractions, recalling information, and adaptively regulating emotions can have far-reaching and devastating effects on goal-directed functioning, undermining success in school, work, and other aspects of personal life. Help from brain injury professionals is vital to preventing these experiences from devolving into a downward trajectory of setbacks and disappointments. There is a great need for intervention research and development focused on the issues most commonly affecting current generation Veterans (Cooper et al., 2015).
One area of critical importance for intervention development is helping individuals regulate their cognitive and emotional states, focused on and guided by their personal goals. The story above highlights the need for interventions that address chronic difficulties, unify complexities of neuro-cognitive-emotional functioning in an individualized goal framework, and empower the individual to improve their wellbeing and achieve their life goals (i.e. taking a strength-based approach). This Veteran’s story also draws attention to the need to minimize gaps in care, helping Veterans ‘where they are.’ In this article, we review a line of work focused on helping individuals better regulate cognitive-emotional states to pursue their goals, discuss our process of using neural biomarkers to test and build a foundation in intervention theory, and describe implications for service delivery. Over the past decade, we have collaborated with Veterans and others to develop tools and approaches for improving goal-directed functioning. We have worked to bring together clinical rehabilitation best practices, cognitive neuroscience, technology, education, and individualized goals to forge innovative pathways to improve brain functions essential to pursuing and attaining goals in the face of challenges. We have adopted a rehabilitation neuroscience approach to developing interventions for real-world application, which involves testing our interventions systematically to examine their practical applications as well as theoretical underpinnings. This work allows for ongoing, iterative improvements and has led to a series of interventions that emphasize intensive guided experiential learning to improve functioning in the lives of brain injured individuals.
Targeting Regulation of Internal (Brain) States Utilizing a Goal Framework
Our goal is to help individuals improve abilities fundamental for learning, adapting, problem-solving, and, more generally, achieving goals in challenging situations (Chen & Loya, 2014; Chen & Novakovic-Agopian, 2012). We argue that impairments with goal-directed functioning are often related to underlying problems regulating internal (brain) states during goal pursuit. At the behavioral level, continuous and dynamic regulation is needed throughout the entire goal pursuit endeavor, from the initiation of goal-directed activities to overcoming potential challenges to goal achievement. At the neural level, modulation of brain states affects signal and noise properties of information processing systems upon which goal-directed functioning is based. Some brain states, reflected in parameters of functional brain networks, may be associated with enhanced learning, memory, and self-control, and this has direct implications for rehabilitation (Arnemann et al., 2015). This foundation has informed our approach to training state-regulation skills (SRS). Improving the goal-directed regulation of brain states is hypothesized to help individuals better achieve their goals by strengthening their abilities to direct and sustain attention toward goal-relevant information, selectively maintain this information over time, manage non-relevant distractions, and re-direct attention.
We argue that for SRS to be effectively learned, training should include at least four key elements (Chen, Loya, & Binder, in press). First, training should facilitate each trainee’s conceptual understanding of trained skills, including the underlying rationale and intended benefits of skill use. Second, training should include opportunities where skill use can be extensively practiced across a wide range of goal contexts and challenges. This may help with skill development and promote automaticity in skill use, increasing the likelihood that a state regulation response will be triggered in-the-moment during any challenge context. Third, training should increase trainees’ awareness of situations where their goal-direction is vulnerable to disruption, and foster their intentions to apply skills in instances when they are most likely to be derailed. Finally, these elements need to be tied together in a goal framework, explicitly supporting the strategic application of SRS to bolster goal attainment efforts. Together, these elements may maximize application of SRS in situations when and where they are needed most.
With these principles in mind, we first designed a group-based experimental intervention protocol for training goal-oriented attentional self-regulation (GOALS; Novakovic-Agopian et al., 2011). The primary focus of training is learning to strategically apply SRS across multiple settings and contexts. Training involves supported practice of a Stop-Regulate strategy, cued using the mantra Stop-Relax-Refocus, during in-session exercises and in relation to personal life goals and individual and group projects. To help guide strategic skill application in a goal framework, participants are instructed in stepwise goal management strategies (Levine et al., 2007). In an initial pilot, 16 brain injured individuals receiving training demonstrated greater improvements on neurocognitive measures of complex attention and executive functions, a real-world functional task, and self-reported abilities relative to a brief educational control intervention. The vast majority of these participants (94%) also reported continued strategy use 2-3 years following training (Loya et al., 2017). Larger controlled studies for Veterans with TBI and TBI-PTS are ongoing; preliminary findings of these studies parallel improvements found in our pilot investigation.
Figure 1
Example scenarios from a progression of cognitive contexts with integrated, parameterized challenges to goal-directed functioning: (a) managing multiple tasks in an executive suite of a corporation, and (b) serving multiple customers as a food truck entrepreneur. Gameplay progresses to managing multiple aspects of the growing company.
Harnessing Technology to Enhance Neurocognitive Skills Training
We next sought to intensify training of SRS by providing a greater range of contexts, with a calibrated progression of challenges for experiential learning. Providing additional active learning opportunities during training may enhance skill learning and facilitate skill transfer to everyday goal pursuit, particularly if reinforced by coaching supported by direct observations and quantification of skill application. This approach is intended to directly address the limited amount of ‘hands-on’ coaching possible in traditional rehabilitation settings.
We therefore developed training systems that support intensified guided learning of SRS via stepwise experiences. This approach integrates skill instruction, interactive coaching, and intensive skill practice across multiple contexts and settings, bridging from digital game-based scenarios to personal life. We developed a series of digital game scenarios drawn from ‘real-life’ situations to increase the intensity of experiential learning opportunities, ensure that targeted brain functions are challenged in a wide range of complex contexts, increase the relevance of skill practice, and provide concrete experiences to guide discussions of skill transfer to personal life. (See Figure 1.) To maximize learning, an underlying neuroscience-informed architecture parameterizes learning challenges, individualizing information load, distraction challenges, and goal complexity all within a narrative arc. Thus, this training system combines guidance with intensive scenario-based experiences to maximize the learning and strategic use of SRS. Game-based learning experiences are extended and applied to personal life goals and contexts throughout training. The intensified skill learning is intended to be a foundation for additional investigations of neural mechanisms that support functional improvements; however, the training system implementation also has practical implications for addressing gaps in rehabilitation care.
What Neural Mechanisms Support Improvements in Functioning?
In order to investigate neural mechanisms that support functional improvements, we have worked with two lines of functional magnetic resonance imaging (fMRI) biomarkers that capture processes of interest (Arnemann et al., 2015; Chen et al., 2011; Chen et al., 2012; Nomura et al., 2010). These two lines reflect complementary aspects of the working brain in terms of functionally integrated networks.
Decoding information from the brain important for goal-direction
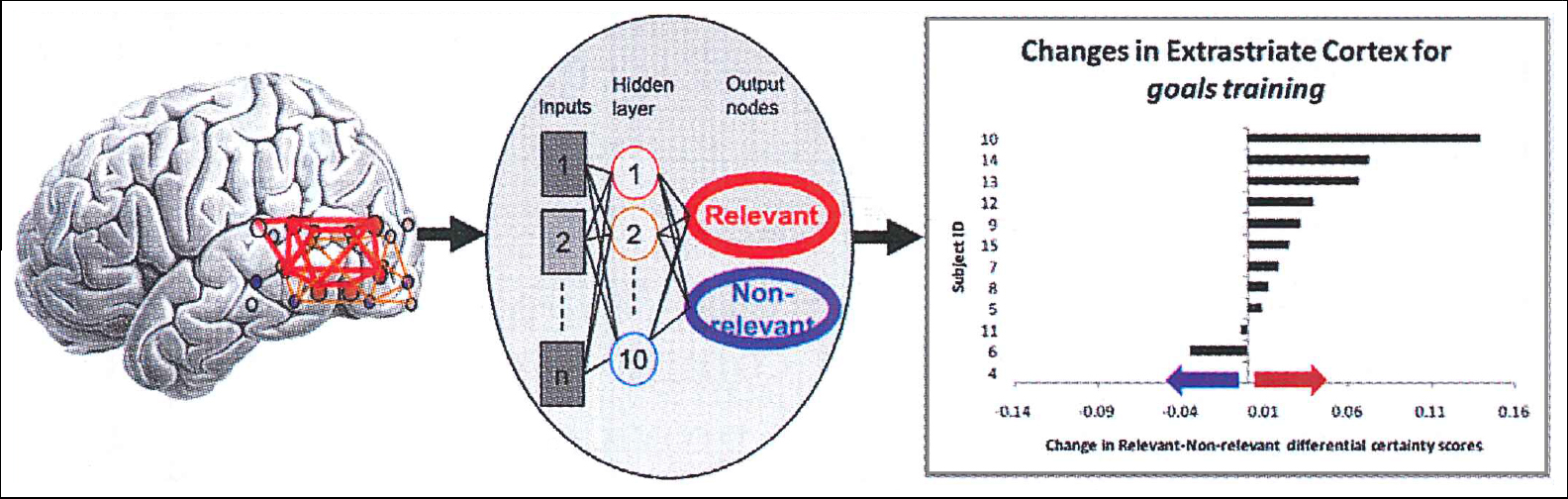
Biomarkers that reflect information coding in the brain’s functionally integrated networks can be informative for longitudinal rehabilitation studies. Our guiding hypothesis is that goal-directed control involves modulation of neural functioning based on goals. The brain fundamentally encodes information in its networks, and thus goal-direction should operate via sharpening the representation of goal-relevant information. That is, greater clarity of neural information codes should logically support goal-directed behaviors. To test the hypothesis that training may increase goal-directed control through this mechanism, we applied measurements that decode information in brain networks. (See Figure 2.) Individuals were scanned before and after GOALS training vs. a brief comparison education activity, and we examined an index of goal-directed control over neural processing during performance of a visual task that required selective information processing. In particular, we indexed the modulation of codes representing relevant and non-relevant information in the visual task. We found an increased modulation of these visual information codes specific to receiving GOALS training. This supports the concept that improved goal-directed functioning could be mediated by sharpening information codes in the brain, a hypothesis worth further testing.
Figure 2: Multi-voxel patterns from functional imaging of posterior brain networks (left) were decoded by a neural network pattern classifier to index processing of goal-relevant (represented by red) vs. non-relevant (blue) visual information (center), with the finding that training resulted in an increased balance of processing of goal-relevant information (right).
Figure 2: How does attention regulation training alter the balance of processing for relevant vs. non-relevant visual information?
Neural markers of ‘readiness to learn?’- Parameters of functional brain network organization as predictors of learning in response to training
Cognitive actions always occur in the context of a pre-existing brain state, and the ability to regulate one’s state likely influences goal-directed cognitive action. Brain state can be described by parameters of functional brain networks such as modularity, a summary of the extent to which a large-scale brain network can be characterized by sub-networks (i.e. modules) vs. being organized with more random or distributed connections. We posit that parameters of brain network state may ‘tune’ how the brain handles tasks, influencing the responsiveness, efficiency and, potentially, the plasticity of brain networks in response to experiences. This may help explain variability that occurs with post-injury rehabilitation. As an initial test, we examined the extent to which individual pre-training brain network modularity might explain variability in response to GOALS training (Arnemann et al., 2015). We found that pre-training modularity predicted the degree of improvement in attention and executive functioning following training, such that higher baseline modularity exhibited greater treatment response. (See Figure 3.) These results support the hypothesis that the regulation of brain network states may influence learning, adding impetus to pursuing training of brain state regulation skills, while also suggesting further investigations of potentially predictive biomarkers.
Figure 3: Functional brain networks from each individual prior to training (example, left) were entered into calculations of modularity (center), and this index was found to be predictive of changes in attention/executive functioning following training (right).
Figure 3
Implications for Service Delivery – Reaching Veterans ‘Where They Are’
While many Veterans (and others) who might benefit from brain injury rehabilitation lack access to care, few research efforts have focused on designing training systems for use in remote settings – in particular, to facilitate intensive skill practice and individualized guidance on skill application. We adapted our technology-assisted training system for televideo implementation. In a pilot study of eight brain injured individuals, participants were highly engaged with training, accumulated significant skill practice in game scenarios, reported benefit in both game and personal life, and showed improvements on measures of complex attention and executive functions.
Reaching Veterans in school is another challenge. Over 1 million Veterans are attending school on the GI Bill, and stigma is one among many barriers to care. Innovative approaches to service delivery are needed to reach these individuals ‘where they are,’ in alignment with their life goals. We have been conducting a pilot investigation of training integrated into the college setting to engage students with TBI-PTS. Feedback and preliminary data have indicated that it is feasible and helpful to offer SRS training in the college setting.
Summary and Conclusions
The effects of TBI on cognitive functioning are complex and have challenged clinicians throughout history, as well as deterred neuroscientists from pursuing studies in this “messy” area of inquiry. The complexity is compounded by combinations of physical and experiential injury. Building a strong scientific foundation is valuable for guiding the development of new therapies. Further, approaches that bridge the basic neuroscience of neural-cognitive functioning with the practical realities of clinical rehabilitation are valuable for intervention development, potentially opening the way for therapies that target biological systems and synergistically augment the specific effects of training. Keeping in mind ongoing learning across the lifespan as a goal of post-injury ‘brain health and wellness’ will expand the horizons for improving the lived experiences of individuals who have suffered brain injury.
References
- Arnemann, K. L., Chen, A. J., Novakovic-Agopian, et al. Functional brain network modularity predicts response to cognitive training after brain injury. Neurology: 84(15), 1568-1574, 2015.
- Chen, A. J., -W. & Loya, F. Mild-moderate TBI: clinical recommendations to optimize neurobehavioral functioning, learning, and adaptation. Seminars in Neurology: 34(5), 557-571, 2014.
- Chen, A. J., -W., Novakovic-Agopian, T., Nycum, et al. Training of goal-directed attention regulation enhances control over neural processing for individuals with brain injury. Brain, 134(Pt 5), 1541-1554, 2011.
- Chen, A. J.-W., Britton, M., Turner, et al. Goal-directed attention alters the tuning of object-based representations in extrastriate cortex. Frontiers in Human Neuroscience: 6, 187, 2012.
- Chen, A. J.-W., Loya, F., & Binder, D. Technological Innovations to Enhance Neuro-cognitive Rehabilitation. In R. L. Kane & T. Parsons (Eds.), The Role of Technology in Clinical Neuropsychology. New York, NY: Oxford University Press, in press.
- Chen, A. J. -W., & Novakovic-Agopian, T. Interventions to Improve Cognitive Functioning After TBI. In J. Tsao (Ed.), Traumatic brain injury: A neurologic approach to diagnosis, management and rehabilitation, (pp. 273-312). New York, NY: Springer, 2012.
- Chen, A. J. -W., Novakovic-Agopian, T., Nycum, T., et al. Training of goal-directed attention regulation enhances control over neural processing for individuals with brain injury. Brain, 2011.
- Cooper, D., Bunner, A., Kennedy, et al. Treatment of persistent post-concussive symptoms after mild traumatic brain injury: a systematic review of cognitive rehabilitation and behavioral health interventions in military service members and veterans. Brain Imaging & Behavior: 9(3), 403-420, 2015.
- Levine, B., Stuss, D. T., Winocur, et al. Cognitive rehabilitation in the elderly: effects on strategic behavior in relation to goal management. Journal of the International Neuropsychological Society: 13(1), 143-152, 2007.
- Loya, F., Novakovic-Agopian, T., Binder, et al. Long-term use and perceived benefits of Goal-Oriented Attentional Self-Regulation Training in chronic brain injury. Rehabilitation Research and Practice, 2017.
- Nomura, E. M., Gratton, C., Visser, et al. Double dissociation of two cognitive control networks in patients with focal brain lesions. Proceedings of the National Academy of Sciences, USA: 107(26), 12017-12022, 2010.
- Novakovic-Agopian, T., Chen, A. J.-W., Rome, S., et al. Rehabilitation of executive functioning with training in attention regulation applied to individually defined goals: a pilot study bridging theory, assessment, and treatment. Journal of Head Trauma Rehabilitation, 26(5), 325-338, 2011.
About the Authors
Anthony J.-W. Chen, MD is on faculty with the Veterans Affairs Northern California Health Care System and University of California, San Francisco (UCSF). Dr. Chen has dedicated the past decade to serving Veterans and others with brain injury through clinical care, innovations in care programs, and neuroscience-driven treatment advancements. He developed a ‘continuum of care’ to support Veterans in their journey from injury to wellness, integrating clinical and research efforts in the Program in Rehabilitation Neuroscience, the Center for Integrated Brain Health and Wellness, and the Successful Transitions and Re-integration Program. Dr. Chen completed Bachelor’s and Master’s degrees in Neuroscience from Harvard and his MD from Harvard-Massachusetts Institute for Technology. He interned at Harvard Beth Israel-Deaconess, received Neurology training at UCSF, and had a fellowship in cognitive neuroscience, patient-oriented research, and cognitive/rehabilitation neurology at UCSF/UC Berkeley.
Fred Loya, Ph.D. is a clinical and research neuropsychologist at VANCHCS. In his clinical work, he provides assessment, cognitive rehabilitation, and psychological counseling services to Veterans with TBI and related comorbidities as part of the interdisciplinary Community Intensive Transitional Re-Integration Program. His research focuses on intervention design and development to address impairments in self-regulation associated with TBI, particularly the integration of digital game technologies into training and the adaptation of training for Veterans with different needs, including students with TBI, and for telerehabilitation. Dr. Loya completed his Bachelor’s degree in psychology from Yale, his Ph.D. in clinical science from UC Berkeley, his internship training at VANCHCS, and his post-doctoral research and clinical training at VANCHCS and VA San Francisco.
Tatjana Novakovic-Agopian, Ph.D. is a clinical and research neuropsychologist at VA San Francisco. Her clinical work involves providing neuropsychological evaluations and cognitive rehabilitation services to Veterans with TBI in an outpatient setting. Dr. Novakovic-Agopian also provides consultations services across the SFVA catchment area up to the border of Northern California. In her research, Dr. Novakovic-Agopian spearheaded the development of the goal-oriented attentional self-regulation (GOALS) training as well as innovative tools for assessing complex, goal-directed functioning in ecologically-valid settings. Her current work is focused on assessing GOALS training for Veterans with comorbid TBI and post-traumatic stress disorder. Dr. Novakovic-Agopian received her doctorate from California School of Professional Psychology and specialty training at Johns Hopkins University and UCSF.
Nick Rodriguez, B.A. has a background in cognitive science from UC Davis. He has been a research associate with Program in Rehabilitation Neuroscience since 2012 and is involved with multiple aspects of ongoing research, including design and administration of experimental tasks measuring working memory, executive functioning and other cognitive abilities; directly training Veterans in longitudinal interventions; and grant administration. He is currently enrolled in a Master’s program in clinical social work through the University of Southern California.
Mark D’Esposito, MD, is a Staff Neurologist and Director of the Neurorehabilitation Unit in the Center for Rehabilitation and Extended Care with the VA Northern California, Professor of Neuroscience and Psychology and Director of the Henry H. Wheeler, Jr. Brain Imaging Center at the Neuroscience Institute at the University of California, Berkeley, and Adjunct Professor of Neurology at UCSF. He received his MD at SUNY Syracuse and completed neurology residency and fellowship at Boston University before joining the University of Pennsylvania in 1993. At UC Berkeley, his lab investigates the role of prefrontal cortex in working memory and cognitive control utilizing approaches such as functional MRI, transcranial magnetic stimulation, pharmacological interventions and behavioral studies of healthy individuals and those with neurological disorders.
Chen, A. J., Loya, F., Novakovic-Agopian, T., Rodriguez, N., & D'Esposito, M. (2017). Using Biomarkers to Discover Pathways to Healing for Veterans with Traumatic Brain Injury. Brain Injury Professional, 14(1), 26-29.
From Brain Injury Professional, an official publication of the International Brain Injury Association and the North American Brain Injury Society. www.braininjuryprofessional.com Reprinted with permission.