Background
Approximately 2.2 million people are currently in US prisons and jails (DOJ 2006). Although women account for about 8% of those incarcerated (DOJ 2006), from 1990 to 2000 the number of women in prisons and jails more than doubled (DOJ 2006). Ensuring the successful community re-integration of prisoners is of concern since approximately 95% of people incarcerated in jail or prison will be released at some point (Commission Report, 2006).
Prevalence and causes of TBI among prisoners
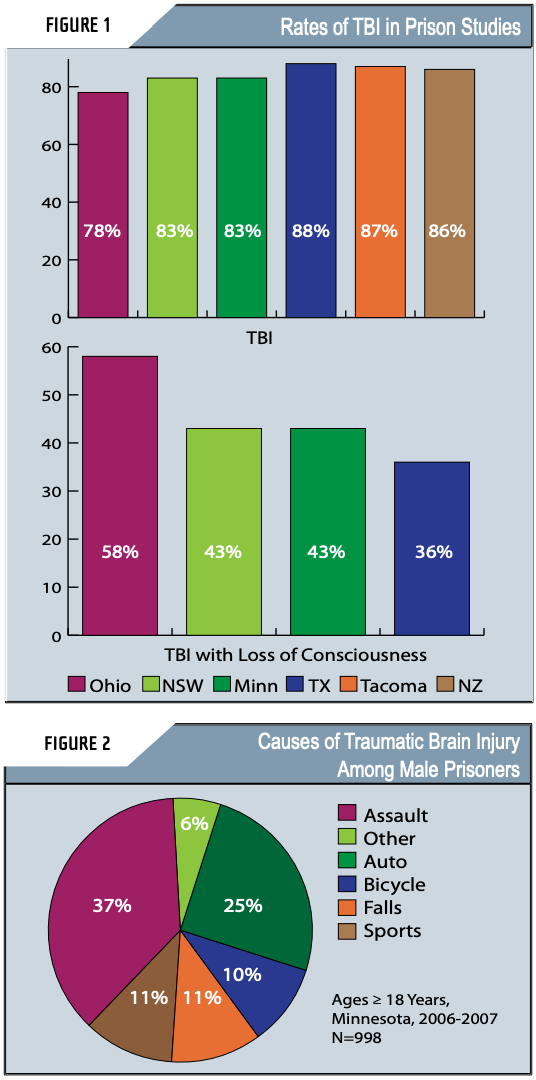
The impact of traumatic brain injury (TBI) in the prison setting has not been well-recognized but is potentially quite great. Previous studies suggest that a history of TBI is common among inmates, including women, occurring among an estimated 25-87% of the jail and prison population (Figure 1). In contrast, it is estimated that 8.5% of non-incarcerated adults report a history of TBI (Silver et al, 2001). These data suggest that the prevalence of a TBI history may be as high as 10 times that of the general population.
Some more recent findings shed new light on the epidemiology of TBI among prisoners. In a recent survey conducted among male state prisoners in Minnesota, a history of having head injury was assessed using the Traumatic Brain Injury Questionnaire (TBIQ) (Diamond et al., 2007). Of the 998 inmates assessed, 82.8% reported having had one or more head injuries during their lifetime, which is consistent with a previous study (Slaughter et al., 2003). The majority were reportedly caused by assaults, followed by automobile crashes and sports (Figure 2). Of note, some of the specific causes of assault-related TBI among prisoners are unique. For example, in the Minnesota project, some of the reported head injuries among incarcerated gang members were the result of a gang initiation procedure called "pumpkinhead" in which new gang members are beaten until their heads swell "like pumpkins." Also, anecdotal reports from corrections officials in South Carolina indicate that self-inflicted TBIs occur when inmates purposely knock their heads against the bars or the cell floor until they become unconscious. This usually happens when inmates are moved to isolated cells (Anbesaw Selassie, DrPH, Medical University of South Carolina, Personal Communication, November 2007).
As an example of how common TBIs are among prisoners, in a recent study of TBI among federal prison inmates, a high percentage of women reported a history of TBI, especially multiple concussions, often totaling 10 or more, and these were usually associated with interpersonal violence (Pamela Diamond, PhD, University of Texas-Houston, Personal Communication, October 2007). One subject in this study estimated that she had been hit in the head and often knocked unconscious by her boyfriend nearly every weekend during a three year period prior to entering prison. According to the study interviewers, many of the women seemed to describe the experience of multiple concussions in a matter-of-fact way, as though they were an expected part of life.
TBI-related secondary conditions
Although a history of TBI is quite common among the offender population, not all TBIs result in long-term disability. The prevalence of long-term problems resulting from these injuries has not been established. However, traumatic brain injury among prisoners is of particular concern because it often results in cognitive, social, emotional, and behavioral problems, including aggressive behavior (NIH Consensus Conference, 1998), and secondary conditions such as substance abuse that can greatly affect their ability to function both while they are in prison and after they return to the community. (Coid, 2005; Merbitz et al., 1995) Knowledge that these problems are related to TBI as opposed to other etiologies would help inform the implementation of TBI-specific interventions, resulting in more effective management and rehabilitation and ensuring greater potential for successful community reintegration.
Individuals with a history of TBI are significantly more likely to have problems with alcohol or other substance abuse (SA) compared with persons without TBI (Silver et al., 2001). However, the relationship between TBI and substance abuse problems among prisoners has not been well-studied. The limited literature to date suggests that cognitive problems associated with a past history of traumatic brain injury (TBI) may affect inmates' potential to succeed in rehabilitation (Valliant, et al, 2003; Corrigan, 1995), including SA treatment (SAMHSA, 1998a).
TBI can result in irritability or aggressiveness, including explosive outbursts, which can be set off by minimal provocation or occur without warning (Silver et al, 2005). Among male prisoners, a history of TBI is strongly associated with perpetration of domestic violence (Cohen et al, 1999), and female prisoners who are convicted of a violent crime are more likely to have had a pre-crime TBI and/or some other form of physical abuse (Brewer-Smyth, 2004). In the prison setting, such aggression and other behavioral disturbances can lead to further injury for the prisoner or others (DOJ 2001; Maryland Police, 2001) and affect corrections center management (Schofield et al, 2006; Merbitz et al, 1995). Aggressive or violent behavior is also associated with recidivism (Coid, 2005). Thus, screening for TBI within the prison setting has been recommended to identify inmates with TBI-related behavior problems and help inform improved inmate safety and management (Schofield et al., 2006). Offenders exhibiting TBI-related aggression might also be taught behavioral and cognitive strategies to inhibit aggressive behaviors (Cohen et al., 1999), although to our knowledge this has not been demonstrated in a prison population.
Although few studies have investigated the topic, homeless-ness has been found to be associated with both imprisonment (Kushel et al., 2005) and with a history of head injury (Bremner et al., 2005), but the role of head injury (or TBI) as a risk factor has not been well described.
Identifying a history of TBI
Screening for traumatic brain injury in prisons has been recommended as a means of informing more effective substance abuse treatment (SAMHSA, 1998b) and inmate management (Schofield et al, 2006; Kaufman, 2005) within corrections facilities.
Anecdotal reports suggest that although some prison intake interviews ask about a history of head injury or TBI, valid and reliable measures for TBI screening have not routinely been used in the prison setting (John Corrigan, PhD, Ohio State University, Personal Communication, July 2006). Results from the recent Minnesota project (see above) suggest that a routine intake question asking if the inmate ever had a head injury was inadequate in identifying head injury. Of the 998 inmates interviewed in that project, only 10 (1 percent) reported a history of head injury during the intake screening, as compared with 826 (83%) who reported having had at least one according to results from the TBIQ, a more detailed screening questionnaire. Similarly, Diamond and colleagues (2007) reported that a one-item, self-administered screener used during admission to prison detected only 19% of the TBIs identified via structured interview. Thus, detailed screening is needed to more accurately identify inmates with a history of TBI.
Some important factors must be considered, however, before screening is begun. First, a good working relationship must be established with corrections officials who initially may have little understanding of the potential importance of TBI within their inmate populations. (Kaufman, 2005) However, their concern for the health and safety of both inmates and corrections officers may be a good starting point for initiating discussions about implementing screening for TBI. Dissemination of fact sheets produced by the CDC, including one specifically aimed at educating criminal justice professionals, could be helpful. (See Sidebar). Second, identification of inmates with TBI should lead to some beneficial action, and establishment of a plan to assist screened populations ideally should be established before screening begins. Some of the potential benefits of screening for TBI among prisoners are that it could lead to improved treatment or management that takes into account the cognitive problems that interfere with the potential of inmates with TBI to adhere to rehabilitation programs designed for persons without TBI. Programs that could benefit from knowledge of a history of TBI include substance abuse treatment, training for victims of violence in strategies to decrease risk, and for perpetrators to manage aggressive behavior, and work assignments, all of which should be tailored to account for TBI-related deficits. Strategies to help victims of violence decrease their risk of re-injury could be implemented. In the long-term, successful implementation of such strategies could lead to more successful reintegration of inmates into work or school, decreased risk of homelessness, and decreased risk of recidivism. Although much more research is needed to design and validate more effective rehabilitation pro grams for inmates with TBI, successful pilot projects could help inform the development of future, more effective interventions.
Once it's decided that a screening program should be implemented, selection of the appropriate screening instrument is important. Selection of a validated screening tool will help ensure that identification is as accurate as possible and help to avoid mislabeling someone as having had a TBI (false positive), or missing a history of TBI (false negative). Two screening tools have been developed specifically for use with incarcerated populations and validation of these measures is currently in progress. First, the Traumatic Brain Injury Questionnaire (TBIQ) (Diamond et al, 2007) is an interviewer-administered instrument with three sections: Section I consists of items asking whether the respondent has ever experienced a head injury from 12 situations associated with such injuries (e.g., vehicle crashes, falls, assaults). Section II probes for details of the head injuries reported in Section I. Questions include age at the time of the injury, whether there was any loss of consciousness or post-traumatic amnesia, and what care was received. Section III assesses the frequency and severity of 15 cognitive and physical symptoms commonly found with head injury (e.g., trouble concentrating or remembering, dizziness or headaches). Of note, inmates are asked about "head injuries" rather than "brain injuries" because the developers of the instrument found that inmates did not understand the term brain injury. The Ohio State University TBI Identification Method (OSU TBI-ID; Corrigan et al, 2007) consists of two steps: Step 1 asks participants to recall any injuries involving a blow to the head or neck or high velocity forces that could have shaken the head violently. Step 2 collects more detailed information about each injury, including whether consciousness was altered, medical attention was received, and if any TBI-related symptoms were experienced after the injury. For both measures, the length of time required to administer them depends on the number of injuries reported. However, the TBIQ takes an average of 15 minutes and the OSU TBI-ID takes about 5 minutes to administer. The OSU Method is also available in a short-form version.
Though useful for identifying offenders with a history of TBI, screening measures are not designed to determine whether specific deficits in function are present. Thus, additional testing may also be needed to identify the smaller sub-sample of inmates with TBI-related deficits who are in greatest need of attention or intervention. For this reason, the Minnesota project is conducting additional testing of inmates who screened positive for a history of TBI using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). The RBANS is a brief screen for assessment of cognitive deficits that has been shown to be useful in evaluating cognitive problems associated with TBI (McKay et al, 2007). With further validation, it is hoped that the OSU method will also provide information that can be used to identify particular characteristics of a history of TBI (severity, age at injury, etc.) that will help identify the inmates who are most in need of intervention. Administration of more detailed neuropsychological batteries may also be needed and helpful if resources are available.
Example of a successful TBI identification pilot project: The Minnesota experience
The Minnesota TBI Interagency Leadership Council (ILC), a public private partnership of agencies, identified behavioral health and criminal justice as areas for development of state capacity with respect to TBI. Various members, especially the Brain Injury Association of Minnesota (BIA-MN), had been contacted by corrections staff seeking service resource information to assist with planning for individuals with TBI. BIA-MN contacted the Minnesota Department of Corrections (DOC) to pursue DOC's potential interest in TBI training and technical assistance. DOC was receptive and training was conducted for DOC staff and, importantly, the agency joined the TBI-ILC. The TBI-ILC then pursued grant funding for a TBI project in collaboration with the DOC.
As a result of these efforts, in 2006 Minnesota was awarded a State TBI Implementation Partnership Grant which is being conducted as an interagency effort entirely through the Minnesota DOC. The three year project, titled "TBI in MN Correctional Facilities: Strategies for Successful Return to Community," is administered by the federal Department of Health & Human Services, Maternal & Child Health Bureau, Health Resources & Services Administration (HRSA). The primary DOC goalsfor this grant include enhancing facility and community safety through identification and effective interventions for offenders with TBI.
The project is currently in the second of three phases. A focus of the initial phase of the project was screening offenders for TBI utilizing the TBIQ. Approximately 1000 adult males, one hundred adult females and fifty juvenile males were screened. (Initial results of those screenings for males are reported in Figure 2). The current phase of the project involves identification of a range of "best practices" interventions that can be used with this population along the continuum of corrections systems and services (i.e., offender management, education, treatment). General information on TBI along with intervention strategies is being broadly disseminated within the DOC through education and training. Development of TBI release planning processes has also begun. In the final phase of the grant, implementation of the TBI identification and intervention strategies will continue along with efforts towards long-term project sustainability.
Conclusion:
TBI among incarcerated populations is an important public health problem. Increased collaboration between traumatic brain injury and criminal justice professionals has the potential to inform more effective management of offenders and increase their potential for successful reintegration into the community. Further research is needed to refine screening methods and develop effective interventions.
About the Authors
Ms. Wald is an epidemiologist with graduate degrees from the Rollins School of Public Health at Emory University and the University of Maryland at College Park. Prior to moving to the Centers for Disease Control and Prevention, she was the Research Program Director for the Department of Emergency Medicine at Emory University School of Medicine where she managed prospective clinical trials and public health studies, including several TBI projects, in three emergency departments including Atlanta's Level I Trauma Center, Grady Memorial Hospital.
Ms. Helgeson is the Project Director for the Minnesota State TBI Implementation Partnership Grant. Helgeson is a Mental Health Program Consultant for the Minnesota Department of Human Services (DHS), the lead state agency for State TBI Grants. She has worked with disability services and policy for DHS for almost 30 years and with brain injury services for over 20 years.
Dr. Langlois is the Guest Editor for this issue of the Brain Injury Professional. She is a Senior Epidemiologist with the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention in Atlanta, GA.
REFERENCES
(Items with an asterisk "*" indicate data sources for figure 1)
*Barnfield TV, Leathem JM. Neuropsychological outcomes of traumatic brain injury and substance abuse in a New Zealand prison population. Brain Injury 1998;12(11):951-62.
Bremner AJ, Duke PJ, Nelson HE, Pantelis C, Barnes TRE. Cognitive function and duration of rooflessness in entrants to a hostel for homeless men. British Journal of Psychiatry 1996;169(4):434439.
Brewer Smyth K, Burgess AW, Shults J. Physical and sexual abuse, salivary cortical, and neurologic correlates of violent criminal behavior in female prison inmates. Biological Psychiatry. 2004;55:2131.
Cohen RA, Rosenbaum A, Kane RL, et al. Neuropsychological correlates of domestic violence. Violence and Victims. 1999;14,397-411.
Coid J. Correctional populations: criminal careers and recidivism. Oldham JM, Skodol AE, Bender DS, Eds. Textbook of Personality Disorders. Washington, DC: American Psychiatric Publishing; 2005: 579-606.
Commission on Safety and Abuse in America's Prisons. Gibbons JJ , Katzenbach NB, co-chairs. Confronting confinement [online]. 2006 [cited 2006 June 8]. Available from: URL: http://www.prisoncommission.org
Corrigan, JD. Substance abuse as a mediating factor in outcome from traumatic brain injury. Archives of Physical Medicine and Rehabilitation 1995;76:302-309.
*Corrigan JD. Unpublished data. 2007.
*Diamond PM, Harzke AJ, Magaletta PR, Cummins AG, Frankowski R. Screening for traumatic brain injury in an offender sample: a first look at the reliability and validity of the Traumatic Brain Injury Questionnaire. Journal of Head Trauma Rehabilitation. 2007;22(6):330-38.
Kaufman CW. Handbook for Correction Officers and Other Institutional Staff to Identify and Manage Inmates With Traumatic Brain Injuries. Ann Arbor, MI: Dissertation Abstracts; 2005.
Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. American Journal of Public Health 2005;95(10):1747-52.
Maryland Police and Correctional Training Commissions. Police interaction with individuals with brain injury: Student workbook [online]. 2001 [cited 2006 February 21]. Available from: URL: http://www.tbitac.nashia.org/tbics/download/mdpolice.pdf
McKay C, Casey JE, Wertheimer J, Fichtenberg NL. Reliability and validity of the RBANS in a traumatic brain injured sample. Archives of Clinical Neuropsychology. 2007;22:91-98.
Merbitz C, Jain S, Good GL, Jain A. Reported head injury and disciplinary rule infractions in prison. Journal of Offender Rehabilitiation. 1995;22:11-19.
*Schofield, PS, Butler TG, Hollis SJ, Smith NE, Lee SJ, Kelso WM. Traumatic brain injury among Australian prisoners: rates, recurrence, and sequelae. Brain Injury 2006; 20:499-506.
Silver J, Kramer R, Greenwald S, Weissman M. The association between head injuries and psychiatric disorders: findings from the New Haven NIMH Epidemiologic Catchment Area Study. Brain Injury. 2001;11:935-945.
Silver JM, Yudofsky SC, Anderson KE. Aggressive disorders. Silver JM, McAllister TW,Yudofsky SC, Editors. Textbook of Traumatic Brain Injury. 2nd ed. Washington, D.C.: American Psychiatric Publishing, Inc.; 2005:259-277.
*Slaughter B, Fann JR, Ehde D. Traumatic brain injury in a county jail population: prevalence, neuropsychological functioning and psychiatric disorders. Brain Injury. 2003;17:731-41.
U.S. Department of Health and Human Services . National Institutes of Health. NIH consensus statement: rehabilitation of persons with traumatic brain injury (October 26-28, 1998). Ragnarsson KT, editor. Washington (DC): Government Printing Office; 1999.
U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration (SAMHSA). Substance Use Disorder Treatment For People With Physical and Cognitive Disabilities: Treatment Improvement Protocol (TIP) Series 29; DHHS Publication No. (SMA) 98-3249; Rockville, MD; U.S. Department of Health and Human Services, 1998a. [cited 2006 July 6]. Available from: http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat5.chapter. 52487
U.S. Dept. of Health and Human Services. Substance Abuse and Mental Health Services Administration. (SAMHSA). Put Prevention into Practice. Treatment Improvement Protocol (TIP) Series 44; DHHS Publication No. (SMA) 98-3249; Rockville, MD; U.S. Department of Health and Human Services, 1998b [cited 2006 August 3]. Available from: http://www.ncbi.nlm.nih.gov/ books/bv.fcgi?rid=hstat5.chapter.80044
U.S. Dept. of Justice. Office of Justice Programs. Bureau of Justice Statistics. Medical Problems of Inmates, 1997. Maruschak LM, Beck AJ (Eds.) Bureau of Justice Statistics Special Report. No (NCJ) 181644. Washington, D.C.; U.S. Department of Justice, 2001 [cited 2006 August 3]. Available from: http://www.ojp.usdoj.gov/bjs/pub/pdf/mpi97.pdf
U.S. Dept. of Justice. Office of Justice Programs. Bureau of Justice Statistics. Prison and Jail Inmates at Midyear 2005. Harrison PM, Beck AJ (Eds.) Bureau of Justice Statistics Special Report. No. (NCJ) 213133. Washington, D.C.; U.S. Department of Justice, 2006 [cited 2006 August 3]. Available from: http://www.ojp.usdoj.gov/bjs/pub/pdf/pjim05.pdf
Valliant PM, Freeston A, Pottier D, Kosmyna r. Personality and executive functioning as risk factors in recidivist. Psychological Reports. 2003;92:299-306.
Acknowledgments
The authors thank Heather Day and Jon Roesler from the Minnesota Department of Health for their assistance in analyzing the data, and Steven Allen and Ken Carlson of the Minnesota Department of Corrections, John Corrigan, and Pamela Diamond for their contributions to this work.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
From Brain Injury Professional, The official publication of the North American Brain Injury Association, Vol.5, Issue 1. Copyright 2008. NABIS/HDI Publishers. Reprinted with permission. All rights reserved.

Comments (1)
Please remember, we are not able to give medical or legal advice. If you have medical concerns, please consult your doctor. All posted comments are the views and opinions of the poster only.
Dawn Quinn replied on Permalink
I was just made aware of my Son having TBI and I will hold the federal prison responsible, this is a tragic event and I will not stop fighting for my Son and find a civil rights lawyer to sue the Federal system