Foreword
By Sarah Jane Donohue
When I was only five days old, the baby nurse my parents hired to help them in my first two months of life shook me so hard, she broke three ribs, both collarbones and caused a severe brain injury. While I lay helpless for over a week, the monster told no one. I was unable to cry, became very lethargic and was finally brought back to the hospital where I was born healthy just two weeks earlier. The monster quickly confessed to her crime and my family was left dealing with the fact that I would never be the same child again.
While being discharged from the hospital several weeks later, the pediatric neurologist told my parents the injury was an eight on a scale of one to 10. When they asked, he said I would never be a normal child and I would probably never walk or talk. The correct answer by this doctor should have been, “I don’t know.” Fortunately for me, my Daddy doesn’t listen to bad doctors!
I was immediately enrolled in Early Intervention and began a rigorous therapy regimen that built up to physical, occupational, vision, feeding/speech therapies and special instruction — up to three hours of each therapy per week! When I was one year old my Daddy created a special crawler which allowed me to move independently. Then, for Christmas that year, he built me my very own walker and he even adapted it so I could walk on the treadmill!
My Daddy read as many books about neuroplasticity and neurology as he could handle (although I think some of the books he just skimmed because they were very complex). The more he read, the more he realized how little was known about the brain at all, let alone an infant’s brain. He also realized there was no single repository of information about neurological breakthroughs or discoveries – it is an extremely fractured field. It reminded him of the computer science industry the 1950s and 1960s, where brilliant people were working all over the world in the same areas, but no one knew specifically what anyone else was doing.
He took that idea and then asked himself, “Where are all the breakthroughs occurring today?” The answer was in Open Source Principles, which is basically the concept of shared knowledge. Since no one was using those principles in the field of neuroscience, Daddy decided to do it himself. He launched The Sarah Jane Brain Project in October 2007, and Phase One entailed putting all of my medical records and videos of my therapy sessions online in an Open Source format – the first time in medical history this had ever been done for anyone.
Phase Two of the Sarah Jane Brain Project involved recruiting other families of children like me who have brain injuries to participate, since the more of us who gather together, the stronger we are. During this phase, he also began to recruit the best in the field of pediatric acquired brain injury to help him develop the first-ever National Pediatric Acquired Brain Injury Plan (PABI Plan). Every family affected by brain injury my Daddy has ever connected with talked about having to reinvent the wheel in learning how to perform basic care and receive basic services for their child instead of being able to focus on the uniqueness of their child’s specific issues.
Phase Three consisted of having the Working Group of the National Advisory Board of the Sarah Jane Brain Foundation develop the first draft of the National PABI Plan. This document is designed to outline a comprehensive continuum of care, from prevention of pediatric brain injuries to acute medical care to reintegration and rehabilitation in the community and transition into adult systems.
Phase Four involves fully funding and implementing the National PABI Plan across the country. My Daddy promised to begin Phase Four before my fourth birthday on June 5, 2009, and he has. While I still cannot talk or walk on my own yet, my Daddy has taught me his philosophy in life, “Things work out best for those who make the best out of the way things work out!” I cannot begin to thank the National Advisory Board enough for being my voice and the voice of the millions of children and young adults around the country who suffer from pediatric acquired brain injury. Someday I will thank each and every one of you myself with my own voice! Until then, please keep talking for me.
Preface
Brain injury is the #1 leading cause of death and disability in the United States for children, adolescents and young adults. Particularly because their brains are still developing, it can result in wide-spread impairments and dysfunction not only in cognition and motor function but also in behavior and social function. The injury can also affect the developmental trajectory which in itself can increase dysfunction or exacerbate impairment. A developing child/young adult’s recovery, rehabilitation and habilitation from a brain injury is a complex process influenced by premorbid child and social environmental characteristics, acute monitoring and treatment, and the responses of family, school, and community during this process. As such, it requires a coordinated interdisciplinary response to facilitate long-term rehabilitation.
The Sarah Jane Brain Project (SJBP) recognizes many of the practices described in this document are currently being implemented. It is the purpose of this document to build on the many individualized practices that exist. However, the consistent availability, coordination and integration of the numerous well-established interventions, programs, and supports do not exist at the present time on a national level. The mission of the Sarah Jane Brain Project is to develop a seamless, standardized, evidence-based system of care universally accessible for all children/young adults and their families regardless of where they live in the nation. This system of care is called the National Pediatric Acquired Brain Injury Plan (PABI Plan). The Sarah Jane Brain Project will facilitate this integration along with ongoing development of effective interventions and supports, and their validation through research guided by theory, existing data across disability populations, and participant needs.
There are many definitions of pediatric acquired brain injury (PABI) and pediatric traumatic brain injury (PTBI). For the purpose of this document, the term PA/TBI will be used. This includes traumatic causes such as those sustained as a result of motor vehicle accidents, sports-related injuries, blast injuries from war, assaults/child abuse, gun shot wounds and falls along with non-traumatic causes including but not limited to anoxia, infection, brain tumor, stroke, seizure, inflammation, toxins, meningitis, substance abuse and metabolic disorders. The focus of the SJBP is on children, adolescents and young adults, ranging in age from birth to 25 who have sustained a traumatic or non-traumatic acquired brain injury. Young adults are included due to the fact that their brains are still developing, as indicated by biological measures (brain metabolism, myelination), neurocognitive measures (executive functions, inhibitions) and social measures (beginnings of independence, transition to adult privileges and responsibilities).
In order to carry out this integrated seamless system of care, the Sarah Jane Brain Family (SJBF) Centers of Excellence will be created. With advances in technology, neuroinformatics and assessment including functional brain imaging and genomics, the establishment of a SJBF Center of Excellence in every state will dramatically improve the lives of children by increasing our understanding of the determinants of rehabilitation from PA/TBI and to inform the development of innovative, empirically-based interventions. Such a system will offer significant cost efficiencies, funding efficiencies and independent revenue models.
The terms recovery, rehabilitation, and habilitation are used throughout these documents and represent overlapping processes. Definitions of these terms are needed, as well as clarification of how they relate to intervention and key reintegration periods (transition from hospital to rehabilitation, reintegration from hospital to home, reintegration into the school system, and transitions into each stage of life).
Recovery is defined here as an ongoing process that begins as soon as the patient is medically stable and continues until the patient no longer shows improvement in any impaired functions. The process continues across acute, sub-acute, and chronic phases. In the acute phase, recovery represents stabilization of neurologic, metabolic, and/or medical status, usually through interventions targeted to brain and body health (i.e., stabilization of intracranial pressure, inflammation, etc.). The use of the term recovery in the sub-acute and chronic phases is used to reflect continuing biological changes in brain function and plasticity. These almost certainly interact with processes of normal brain development.
Neuroimaging research in humans suggests these recovery processes may continue for years after injury. The end of the acute recovery process is determined when the effects of injury on cognition, mood, and behavior can begin to be most accurately assessed. However, recovery may not occur spontaneously and should be actively promoted through rehabilitation and habilitation.
Rehabilitation in this document is intended to represent periods of active intervention that might include but are not limited to: pharmacological, physical, occupational, vision, speech-language, psychological, behavioral, and/or educational therapies. Rehabilitation should continue as long as it results in improvements in function. When interventions no longer yield improvements in function, the child transitions into a period of habilitation.
We must acknowledge these periods are not clearly definable stages nor do they necessarily occur along a continuum. The entire process of recovery from injury will include multiple periods of active rehabilitation interspersed with periods of habilitation as new concerns are identified such as when children transition from one stage of life to another. The key is initial identification of brain injury, control of the cascade of injury processes during the acute phase, and active surveillance to identify any developmental stalls or new concerns.
In addition, while a TBI may be classified medically as “mild,” the term can be misleading since there is nothing “mild” about any brain injury, thus the reason for quotation marks around the word throughout the document.
Principles for SJBF Centers of Excellence
Once the SJBF Centers are in operation, they will be guided by four over-arching goals:
- To prevent PA/TBI through changes in social practices and policy.
- To facilitate the provision of care and services to maximize the child/young adult’s recovery and development after PA/TBI and to support the family though all stages of recovery.
- To improve the capacity of schools and community agencies to deliver rehabilitative and educational services and support to the child/young adult and family.
- To use research to better understand the effects of neurological insults on the developing brain, to research the individual, medical and social environmental determinants of recovery and function, as well as the most effective interventions for improving child/young adult and family outcomes.
These centers will serve not only as primary, secondary and tertiary care facilities but also as resources for individual physicians, caregivers, families and other hospitals (see Figure 1). Data will be incorporated into a centralized SJB Family Registry (see Chapter 7), allowing for the efficient evaluation of best practices. Findings from research will be disseminated using methods developed by the SJBP to share knowledge gained with the entire brain injury community. The specific principles underlying these goals are outlined below.
Principle 1: Prevention is the best possible treatment for any brain injury and includes preventing the initial insult as well as preventing secondary medical, social, and behavioral consequences, including preventing a second injury.
Principle 2: The developmental stage of the child/young adult at the time of injury and recovery across the lifespan must always be considered, and all treatments and interventions should be implemented by individuals with pediatric training and special expertise in PA/TBI.
Principle 3: Providers and all professionals should adhere to the principles of family and person-centered care, engaging the family and child/young adult themselves in a collaborative process for setting and achieving treatment goals.
Principle 4: Early identification of PA/TBI is critical to improving long-term outcomes.
Principle 5: Best clinical practices need to be determined based upon evidence from research and then standardized to be effective and efficient.
Principle 6: Children’s recoveries are strongly influenced by their environmental contexts (home, school, community). Beyond early hospitalization, interventions to improve outcomes for children and young adults with PA/TBI must occur in the settings in which children and young adults with PA/TBI live and function (school, home, and community), and must involve the “everyday people” in these settings such as parents/caregivers, teachers, and peers.
Principle 7: Interventions for children and young adults with PA/TBI must acknowledge
the overlap among different disability populations in terms of treatment needs and useful
interventions.
Principle 8: Research should use a variety of methodologies to examine hypotheses
regarding recovery and intervention (prospective, naturalistic follow-up studies,
randomized controlled trials, single subject experiments, qualitative studies, and animal
models).
Principle 9: Interventions for children with PA/TBI occur at multiple levels (e.g., physical, medical, psychological, family, school, community) and across a continuum of care (e.g., acute care, rehabilitation, re-entry, and ongoing educational, social, and vocational life). Research on the effectiveness and efficacy of intervention should link both vertically (i.e., across levels) and horizontally (i.e., across the continuum of care), must follow children and families long-term, recognize that needs are likely to change over time, use functional outcome measures, and measure generalization to a variety of functional contexts of application.
Principle 10: Interventions for children with PA/TBI occur across a developmental spectrum that varies according to age at injury, time since injury, and age at intervention. The effectiveness and efficacy of any intervention may vary as a function of these developmental parameters because of critical variations both in neural developmental and environmental contexts.
Principle 11: Proper PA/TBI training and education for future medical and educational professionals should be integrated into current graduate and medical school programs in order to ensure continuity of care is taught to those just entering the medical or educational profession.
Executive Summary
Pediatric Acquired/Traumatic Brain Injury (PA/TBI) is a national disaster. Because a brain injury is typically “invisible,” it remains unrecognized or under-recognized, thereby markedly increasing the burden of care in all aspects of society. The effects of a PA/TBI are complex and require the integration of medical, educational, judicial and social service systems.
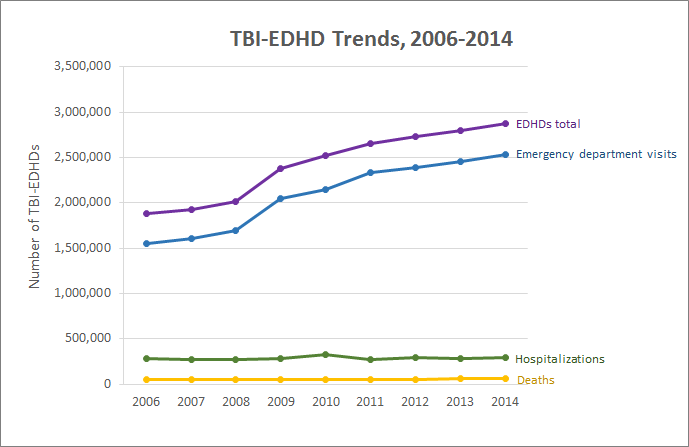
PA/TBIs are truly an epidemic. The Centers for Disease Control and Prevention (CDC) reports that for children aged 14 and under there are 2,685 deaths, 37,000 hospitalizations, and 435,000 emergency room visits attributable to TBI annually (see Figure 2). As the incidence of PA/TBI is at its maximum for those aged 16 to 24 years, and due to the fact that not all individuals with TBI present to an acute care hospital, these staggering numbers can only be underestimates of the true rates of PA/TBI.
The World Health Organization (WHO) has noted that PTBI is the NUMBER ONE cause of morbidity and mortality for children and young adults. Children are 20 times more likely to die from PTBI than from asthma and 38 times more likely to die than from cystic fibrosis. Additionally, the WHO reported in 2008 that there were twice as many children who suffered a brain injury than those who received stitches.
The financial burden of PTBI is estimated to cost well over $12 billion a year (2000 CDC data). This figure does not include the significant financial impact of those children and young adults, who because of their PTBI will never be able to contribute financially or otherwise to society as adults, nor does it include lost productivity of the child/young adult’s parents and family. These numbers also do not include those children who acquire their injuries from non-traumatic causes such as stroke, brain tumors, infections of the brain and anoxic/hypoxic injuries.
While the economic cost of PA/TBI is clearly underestimated and growing every year, the positive impact of enacting the National PABI Plan is clear. Since there is a huge decrease in lifetime earnings and other outcomes such as educational achievement of children/young adults with PA/TBI, any positive improvement in functioning and contributions to society has an enormous compounding impact. In addition, since the SJBF Centers are focused on supporting families as well as the child/young adults, the exponential increase in productivity of the parents/caregivers over time as a result of that support is staggering. Since most parents become the primary caregivers/case coordinators for their children, this becomes another distinguishing difference between the adult ABI and PA/TBI population.
Since these SJBF Centers will be gathering considerable quality information through a specially designed registry, it will be possible to examine the economic benefit from a treatment or care management plan, whereby changes in said earnings could be measured compared to their counterparts that do not receive such treatment. It will be possible to combine the estimates of the change in the cost of care based on such treatment. Some potential outcomes to consider include the additional savings per life saved, the additional savings per life year gained, the additional net economic savings per life year gained, the additional savings per quality adjusted life year (QALY), the additional net economic benefit per QALY gained and the net economic benefit of any particular intervention. These types of economic analyses are currently unrealistic because of the dearth and quality of data.
For the families who have experienced a child/young adult with a PA/TBI, it is a terrifying and challenging experience. Their children are often not diagnosed and many are misdiagnosed. Access to comprehensive and integrative care is extremely rare. Most troubling, ongoing and coordinated support for the lifetime needs of someone with a PA/TBI is virtually nonexistent. Families have to be constantly searching and reinventing services because there is no coordinated, seamless circle of care for those with PA/TBI or their families.
Historically, PA/TBI has been studied and addressed primarily as a medical issue. Program development has taken place largely at the level of medical rehabilitative treatment. Most of the research has focused on this level of treatment as well as on children’s outcome from the perspective of their neurological impairments. However, a number of important considerations mandate a sharpened focus on long-term issues from psycho-social, educational and environmental perspectives, as well as increased support for ongoing rehabilitative, educational, and support services provided by the school systems and other community providers.
The school systems are now acknowledged to be the major provider of rehabilitative as well as educational services for children and adolescents with PA/TBI. Following a severe brain injury at age 10, for example, a child/young adult may receive services for three months in acute and rehabilitative medical care, followed by eight years of services in the school system, a ratio of 1:32. Investigators agree that rehabilitative needs evolve and often grow in number and intensity over the years after PA/TBI, resulting in seriously compromised adult outcomes.
Furthermore, because school professionals have less training than medical and rehabilitation professionals in understanding and managing PA/TBI-related issues, their need for training and support is greater than that of medical and rehabilitation professionals. Fortunately, the few studies that exist suggest that well-conceived interventions and supports delivered after discharge from medical rehabilitation can be effective, significantly benefitting the child/young adult, family members and education staff.
For all of these reasons, the SJBF Centers of Excellence will provide leadership in designing, studying, and disseminating long-term interventions and supports for children with PA/TBI and their families, delivered by effectively trained and supported community professionals.
Sarah Jane Brain Project (SJBP):
In an effort to address this major gap in care, the SJBP organized and consulted with the Working Group of its National Advisory Board. These experts in the field of PA/TBI have over 1,000 years of collective experience and their task was to analyze the continuum of care for PA/TBI, identify the problems along this continuum and then propose solutions. As a result of this effort, the National PABI Plan was drafted and made public along with the first letter sent to President Barack Obama on January 20, 2009, at 12:01 p.m.. What follows is the final version of a suggested comprehensive, integrative, accessible, culturally sensitive, long-term and child/family centered circle of care for PA/TBI. These experts included families and family advocacy organizations, physicians, allied health care professionals, educators and researchers.
Wherever possible, these recommendations are based on evidence derived from "good" science. However, there is little research being done in the broad field of PA/TBI in comparison to the magnitude of the problem. We have identified key research questions that must be addressed immediately to improve the management and long-term treatment of PA/TBI. There were two key research components examined by the Working Group along the continuum: 1) translational research — “What are the questions needed to be asked and what data needs to be gathered to ensure the PABI Plan is tested, evidence-based, and replicable?” and 2) basic science research — “What are the questions needed to be asked and what data needs to be gathered to advance the field of PA/TBI?”
The long-term research agenda of the SJBF Centers will be formed by emerging clinical and research evidence and reflect an interdisciplinary integration of research questions and methodology. It should be noted this research agenda is by no means complete, but does represent the areas of research that can provide the maximum help in the management of PA/TBI as quickly as possible with future research needs to be delineated over time. Indeed, the entire circle of care will need to be modified as more evidence of best treatments is documented.
For the purposes of this position paper and overall initiative, the expert working group recognizes that Traumatic Brain Injury (TBI) is a subset of Acquired Brain Injury (ABI). As such, to ensure that there is no gap in the discussion, issues, and services between these areas of Pediatric Acquired Brain Injury (PABI), the terms are being combined and will be herewith referred to as Pediatric Acquired/Traumatic Brain Injury (PA/TBI). This group of experts was divided and asked to address (1) prevention, (2) acute care needs, (3) transition to the community and ongoing rehabilitation, (4) long-term needs, (5) research which will span all phases and (6) child/young adults, parents/caregivers, siblings and other family considerations at each stage. Where necessary, the severity and cause of the PA/TBI was also addressed.
In addition, the definition of PA/TBI takes into consideration and includes the age range from birth to age 25 years because of the recognized physiological developmental changes that the brain is still undergoing in the third decade of life. As such, it encompasses the care of over 73.3 million children and young adults within the United States of America based on the 2000 census.
The PABI Plan has been developed into seven “Categories of Care” for treating brain injuries in children and young adults: 1) Prevention, 2) Acute Phase, 3) Mild TBI Assessment / Treatment, 4) Reintegration / Long-term care, 5) Adult Transition Phase, 6) Rural / Telehealth and 7) The Virtual Center. For each Category of Care, it will be important to establish a nationwide standard for collecting translational data, a standard set of training, education and dissemination of information, and the ability to monitor and develop basic science research.
The entire program is based on the following premise: the most important way to treat PA/TBI is to prevent it in the first place. Prevention has been conceptualized broadly to include programs that are available to prevent PA/TBI caused by everything from motor vehicle collisions to programs addressing other forms of acquired brain insult such as those to encourage sound immunization regimens and improved nutrition.
Prevention occurs at a number of different levels including primary prevention which entails forestalling PA/TBI in the first place, secondary prevention which involves limiting the impact of PA/TBI, and tertiary prevention, or preventing repeat brain injury. Prevention programs must be evaluated to prove they make a difference and actually decrease the incidence of PA/TBI. Existing programs that have been or are being shown to be effective should be expanded and instituted nationwide, when replicable. New programs should be developed, based on evidence, to increase the dissemination of prevention information and this information should be widely distributed.
Education is also a key part of the circle of care. Education should address important aspects of PA/TBI, including: definition, prevention, diagnosis and treatment, facilitation of recovery, provision of needed assistance in schools and participation in the community. Education must target children and young adults, parents and extended family, educators, health care providers across the continuum, and mental health specialists to optimize appropriate identification and treatment over time. Those providing direct services to children/young adults with PA/TBI and their families must be well informed. Although there are many with expertise throughout the nation, the current accessibility to these experts and their overall numbers are insufficient to address the full scope of the problem.
Mild TBI is the largest sub-group with estimates of 1-3 million new children/young adults annually suffering from this largely undiagnosed and untreated condition. In addition to the problem of under-identification, few specialty outpatient clinics exist for active treatment and management. Contributing to this problem, few trained pediatric clinical specialists are available with a focus on “mild” TBI. Hampering service, evidence-based models of pediatric “mild” TBI care are not articulated and therefore, clinicians do not have clear guidance regarding the development of these clinical care systems within the continuum. With a shortage of specialized clinics to treat “mild” TBI and the requisite professional expertise, a variety of problems are evident. Most importantly, without a specialty system in place, the clinical problems that children and families face post-injury are at increased risk for worse outcomes including reinjury, prolonged recovery, and possible catastrophic outcomes.
The SJBF Centers will seek to standardize acute care for PA/TBI during field-side assessment, Emergency Department triage and stabilization, critical and acute care management in hospital and rehabilitation based on state-of-the-art evidence. This standardized approach must encapsulate all areas of healthcare delivery and healthcare personnel education/training. In addition, the Centers will emphasize the importance of timing rehabilitative interventions appropriately in the care of the child/young adult with a brain injury. Ongoing research is essential and will be conducted in the best way to care for children with PA/TBI, and as new information emerges it will be disseminated to other sites as rapidly as possible. Each Center will have exceptionally-trained Sarah Jane Brain Family (SJBF) Specialists who will operate as “super-caseworkers” for each family.
Rehabilitation begins during the acute recovery phase and can continue throughout the child or young adult’s life. The SJBF Centers will seek to expand our understanding of how much, what kind and when rehabilitation is necessary for various kinds of PA/TBI. Communication with the family and the initiation of the transition the family will undergo is imperative. Initiating rehabilitation programs early is paramount, but so is the recognition that the rehabilitative process continues in the child/young adult’s community and this rehabilitation needs to be ongoing as the child/young adult develops and grows and the brain undergoes the physiologic preplanned growth and refinement necessary for brain maturation. Indeed, one of the reasons why PA/TBI is so different from adult A/TBI, is the fact the brain is maturing and new skills are emerging. Infants, children and young adults often manifest their PA/TBI when they fail to meet expected developmental milestones at the appropriate times.
It is equally important to recognize that transitioning from the pediatric system into the adult system of care is one of the most difficult and challenging phases. There is a need to coordinate the transition for individuals, caregivers, educators and the community since the adult system of care is more directed towards independent living and vocational training without the structured support system of the ideal pediatric system. There is very little research done within the Adult Transition Category of Care.
In order to develop a system of care that is universally accessible for all children/young adults and their families no matter where they live in the nation, it is imperative we have an emphasis on the families living in rural America, which encompasses over 75% of the landmass in our country and almost 25% of our population. In order to accomplish this mission, telehealth and telerehabilitation programs must be developed, tested and implemented throughout the country.
In order to standardize the system of care, evidence and data will be collected, analyzed and stored through The Virtual SJBF Center. In addition to serving as a data collection pool, the Virtual Center will be an online resource for individuals, families, professionals and the general public for all stages of the continuum of care and an opportunity to use advancements in healthcare I.T. to improve the system of care.
Sarah Jane Brain Legal Center:
An additional component of the National PABI Plan is the Sarah Jane Brain Legal (SJBL) Center. The purpose of the SJBL Center is to provide children and adolescents with the best means of accessing the supports and services necessary for individuals with PA/TBI. The legal center will incorporate education about and the most effective means for obtaining these services from the medical, educational and social services communities or organizations, as well as other legal entities, in the most efficient manner. Always taking into consideration the needs of the child/young adult and family, the legal center will ensure a continuum of service delivery into, through and beyond the legal age for those services. The legal center will serve as a legal hub for any legal issues the child/young adult and family needs and also facilitate appropriate transition and access of services into the adult world and support continuity of those services.
The National Advisory Board has also begun looking at long-term revenue models so the system of care is not solely reliant upon public financing. The Sarah Jane Brain Legal Center will serve as one source of non-public funding. In addition, The Sarah Jane Brain Foundation will develop its own contract research organization (CRO) focused around pediatric acquired brain injuries which should be able to generate significant funding for the system of care over time as well and generate additional research projects. There are numerous other revenue and fund-raising plans which are in the process of being developed. We expect non-public revenue to eventually become the largest component of our budget.
Read the whole National Pediatric Acquired Brain Injury Plan.
From the National Advisory Board of The Sarah Jane Brain Foundation. Used with permission. www.thebrainproject.org.