
If you’re experiencing post-traumatic stress disorder (PTSD), it’s important to understand how the different parts of your brain function. Post-traumatic stress is a normal response to traumatic events. However, PTSD is a more serious condition that impacts brain function, and it often results from traumas experienced during combat, disasters, or violence.
Your brain is equipped with an alarm system that normally helps ensure your survival. With PTSD, this system becomes overly sensitive and triggers easily. In turn, the parts of your brain responsible for thinking and memory stop functioning properly. When this occurs, it’s hard to separate safe events happening now from dangerous events that happened in the past.
Over the past 40 years, scientific methods of “neuroimaging” have enabled scientists to see that PTSD causes distinct biological changes in your brain. Not everybody with PTSD has exactly the same symptoms or the same brain changes, but there are observable patterns that can be understood and treated.
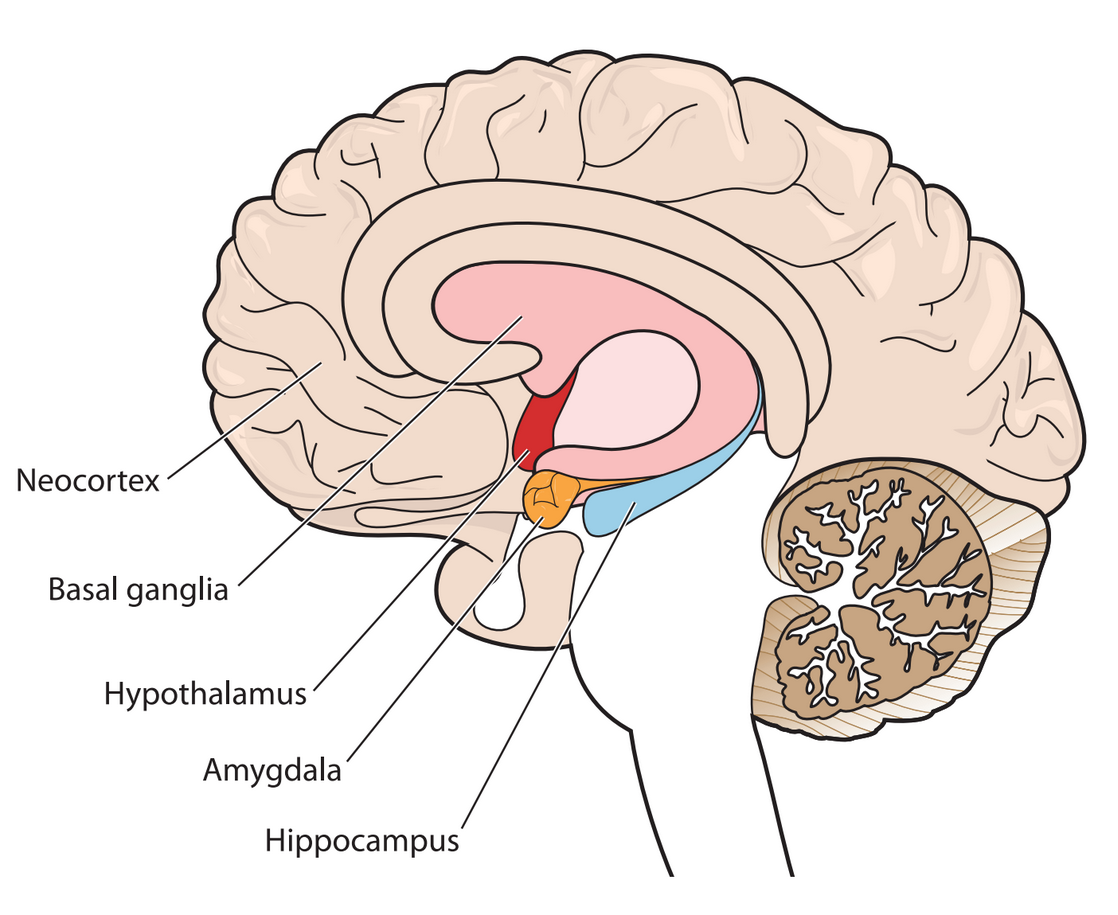
The diagram shows a cross-section of the brain parts discussed here.
Your alarm system
Your amygdala triggers your natural alarm system. When you experience a disturbing event, it sends a signal that causes a fear response. This makes sense when your alarm bells buzz at the right time and for the right reason: to keep you safe. Those with PTSD tend to have an overactive response, so something as harmless as a car backfiring could instantly trigger panic. Your amygdala is a primitive, animalistic part of your brain that’s wired to ensure survival. So when it’s overactive, it’s hard to think rationally.
Your brake system
Your prefrontal cortex (the front-most part of your neocortex) helps you think through decisions, observe how you’re thinking, and put on the “brakes” when you realize something you first feared isn’t actually a threat after all. Your prefrontal cortex helps regulate emotional responses triggered by the amygdala. In service members with PTSD, the prefrontal cortex doesn’t always manage to do its job when needed.
A bad combination
An overactive amygdala combined with an underactive prefrontal cortex creates a perfect storm. It’s like stomping on your car’s accelerator, even when you don’t need to, only to discover the brakes don’t work. This might help you understand why someone with PTSD might: (1) feel anxious around anything even slightly related to the original trauma that led to the PTSD; (2) have strong physical reactions to situations that shouldn’t provoke a fear reaction; and (3) avoid situations that might trigger those intense emotions and reactions.
System recall errors
Other common PTSD experiences—such as unwanted feelings that pop up out of nowhere or always being on the lookout for threats that could lead to more trauma—seem to be related to the hippocampus, or memory center of your brain. Your hippocampus is a lot like your computer’s memory that writes files to its hard drive. After a trauma, your hippocampus works to remember the event accurately and make sense of it. But because a trauma is typically overwhelming, all the information doesn't get coded correctly. This means that you might have trouble remembering important details of the event, or you might find yourself thinking a lot about what happened because your hippocampus is working so hard to try to make sense of things.
Debrief/Bottom line
Your amygdala, prefrontal cortex, and hippocampus all contribute to the feelings and actions associated with fear, clear thinking, decision-making, and memory. Understanding how they work also might explain why some therapies can help you work through PTSD. For a visual guide to these and other parts of your brain, and more information about them, explore the Center of Excellence for Medical Multimedia’s “Interactive Brain.
How PTSD affects brain “circuitry”. USU | CHAMP, Human Performance Resource Center, 30 May 2017.

Comments (47)
Please remember, we are not able to give medical or legal advice. If you have medical concerns, please consult your doctor. All posted comments are the views and opinions of the poster only.
Renee' replied on Permalink
I've just been diagnosed with
C-PTSD and I will be 60 years old soon this year. From 1 & 1/2 to 7 years old I was in 9 foster homes. At 7 yrs old I got adopted but I was emotionally disturbed and withdrawn. My parents that adopted me, my mother, physical and mentally abused me. My Father was my protector and would stop her even though he also got abused by my mother that I witnessed many times. I also had a brother adopted with me that got the same treatments from my mother I also witnessed. Once I thought she killed my brother because she knocked him unconscious. At times, my mother waited for my Dad to go to work and then she would beat me and then make me lie to my dad when he saw bruises on my face. I also made me lie when she caused me to get stitches above my right eye to the hospital doctor and my Dad. She got me to lie when she injured me by telling me that she was a diabetic and if I told on her, my sweet father would go to jail in her place because they don't put sick people in jail, I was 8 yrs old and believed her. I suffered from her beatings and terrible words to me that my brain kept filed away until I turned 18, and left home. It doesn't matter how far away you are from the traumas you went through because your brain stores it all not to mention having a broken spirit and broken heart. My sweet and precious Dad just died this past winter. I'm the only surviving immediate family member left. My dad's death "triggered" all my traumas to come forward because I lost my protector, my hero, my prescious dad. I got diagnosed this spring and I've been in therapy. I will be beginning the "EMDR" now that my severe panic attacks are stable. I'm feeling so much better, I never new just how bad off I was. I knew I had depression and anxiety but not what I have been suffering with.
Please, if anyone reading this, and you have been suffering from past traumas or suffering now, don't wait as long as I have to seek help.
Anonymous replied on Permalink
Hello
What therapies do you suggest for PTSD?
Ty
Anonymous replied on Permalink
Very good article, I learned much. I never had any training on this, I retired LE, knew I had to go, I went hard core which isn’t me. I’m still having problems, I can’t make the basic decisions which are easy, only occasionally it happened, but no one needed my wrath.
. replied on Permalink
What are the tests that the article is based off? I’m wondering for a school task
Brett replied on Permalink
Post-traumatic stress disorder (PTSD) can have a significant impact on the brainworks.center PTSD is a mental health condition that can occur after experiencing or witnessing a traumatic event, such as combat, sexual assault, or a natural disaster. Here are some ways that PTSD affects the brain:
Changes in the amygdala: The amygdala is the part of the brain that plays a role in emotional processing and fear responses. People with PTSD tend to have an overactive amygdala, which can lead to increased feelings of anxiety and fear.
Hippocampal shrinkage: The hippocampus is the part of the brain that is responsible for memory and learning. Studies have shown that people with PTSD may have a smaller hippocampus, which can affect their ability to process and remember new information.
Changes in the prefrontal cortex: The prefrontal cortex is part of the brain that is responsible for decision-making and regulating emotions. People with PTSD may have decreased activity in this area, which can lead to difficulty with emotional regulation and impulse control.
Alterations in neurotransmitters: Neurotransmitters are chemicals in the brain that help to regulate mood and other functions. People with PTSD may have imbalances in certain neurotransmitters, such as serotonin and norepinephrine, which can contribute to symptoms such as depression and anxiety.
Overall, PTSD can have a profound impact on the brain, affecting various areas that are critical for emotional regulation, memory, and decision-making. Understanding these changes can help with the development of effective treatments and therapies for PTSD.
Anonymous replied on Permalink
Grateful for this information. I'm currently in therapy dealing with CPTSD. Learning more about the brain has been immensely helpful. Thank you
Nisha replied on Permalink
I went though something similar, even though it may be helpful for you understand the science and psychology of it all. The best treatment is to feel what happened to you, and allow the emotions to come up. Its a lot of hard work and it will be a long process, but that is the only way you can overcome and release the trauma. Other things that help are EMDR, somatic experiencing and yoga.. talking therapies generally dont help (in my opinion).. best of luck for your journey :)
Anonymous replied on Permalink
I want to add that bullying and friendships and relationships ending really badly can also cause PTSD.
Mike replied on Permalink
This is really important to understand how bullying can result in PTSD. People especially in school and in the workplace think its okay to bully, like its part of life. I've been bullied in school, outside of school and in the workplace. I was left feeling extremely anxious, paranoid and angry. I went into a new workplace and felt "triggered" and actually PTSD left me feeling confused about how to behave normally!
Ellen Richardson replied on Permalink
You are so very right and spot on... It seems that it can damage a person for life.
Anonymous replied on Permalink
God bless you all and thank you for your service!
Anonymous replied on Permalink
This is going to sound far-fetched since most people in the comment section are a lot older than me but I am a 15-16 year old who just got diagnosed with ptsd after having it life-long in the fall of 2021. All the things described make so much sense. I know a good amount of things about anatomy and the human body but I did learn a little bit more by reading this. I was abused severely growing up, r*ped and sexually assaulted at a very young age by my dad and r*ped by my step brother at 13. So many things have happened being grown up by a bunch of drug addicts that it has caused me a lot of mental issues including the ones I’m so far knowing of as ptsd, severe depression disorder, anxiety disorder, higher stress levels, adhd, insomnia caused by ptsd and adhd which I’ve had for as long as I can remember, abandonment issues, learning disability associated with numbers and equations, and others I can’t think of at the moment. All these things together definitely cause a tremendous storm. I know it’s going to be a life long hassle but that’s why I’m trying to learn more about each little thing as I go. That’s not even the full list of mental diagnoses and that’s not including any of my physical issues. Thank you for reading. Have a wonderful day!
Anonymous replied on Permalink
I am so sorry that you had to go through so much trauma. I would like to tell you how I was able to get through my PTSD. I listened to calming meditation music on Youtube. I got in touch with nature by walking in the park and also looking at youtube videos that dealt with nature. I read the Bible to help heal my Soul. Forgiveness will also help you to get through PTSD. You have to forgive everyone that caused to harm so you can find Peace within. If you hold on to anger and resentment you won't find peace. I also did deep breathing in the morning and at night. Deep breathing will help you to relax and feel calm. Youtube has deep breathing videos.
Troy replied on Permalink
My friend, don't lose because The Lindner Center of Hope in Cinti, oh is One The Nations Behavioral Hospitals. I had nearly 100 percent of your diagnosis, except the sexual abuse. Go to the website and review the entire website at least three times that you understand to the degree of comprehensive care they give of which the first step is getting properly diagnosed because I suspect that you haven't been diagnosed correctly because some of your symptoms and diagnoses are complex they're multi-factorial and therapists unless you're out in the east it is rare that somebody in the midwest except for lender can I identify these problems thus present treatable Solutions. Then they have some of the world's best specialist including Dr Peck who is more published than virtually anyone in the world with regard to bipolarity disorders look him up moreover there are very few Healthcare institutions that effectively treat obsessive compulsive personality disorder not obsessive compulsive disorder where you want to align your Soup cans outward by subject matter ocpd is when you have the perfectionist syndrome where you have to be at 10 and everything you do to the point where you become paralyzed analysis paralysis and get into the circle of becoming frustrated fatigued depressed you lose interest in everything else is sleep it's a horrible horrible thing to have Leonard uses Innovative therapies like rapid open DBT therapy not your standard DBT or CBT therapy rodbt is for those where meds nor CBT or DBT have worked effectively and believe it or not within 6 months the outcome results show upwards of 60 to 80% Improvement I'll take 10 all day long also along with those CD I have bipolarity matters both of which in addition to depression date back to the 1870s believe it or not the lender Center of Hope Has Affiliates around the world including the Mayo Clinic Johns Hopkins Harvard McLaren which is the best or one of the best in America for mental health care treatment and others I was allowed to participate in a bipolarity study for Mayo Clinic and when you're affiliated with the types of organizations like mayo or others around the world that's how good you are and obviously the PTSD that you're describing right now I am at def com one level to where it is severe I'm having panic attacks all the time I can't breathe my anxiety level severity is borderline severe it PTSD screws with your cognitive and memory functions affects your hippocampus your frontal lobe your parietal lobe all involved in cognitive thinking and emotions look at the dissection of a brain and what each does the parietal lobe gets involved with things like your ability to do math your ability to write your frontal lobe has everything to do with memory and personality concentration and your hippocampus some of that as well and if you drink or do drugs it makes it even more complex but again if you take the time to invest look at the website University of Illinois Chicago Rush Memorial Hospital the Cleveland Clinic if you're out east Johns Hopkins McLane and some in New York City but I would certainly recommend Ro DBT as part of your requirements list it was developed by Dr Marsh from the UK 20 years ago and that's where the experts from the United States look to curing many of these disorders we have good luck and I know you can do it my optimism a year ago was level 2 of 10 now it's an eight because I have a plan I found the right people to do it whereas most and I mean 98% of the sufferers just go to some online program or the mental health facilities out there that ain't going to work
Myss Truman replied on Permalink
I’m so sorry you had to endure all of those terrible experiences. Keep learning about the brain and body and how it was made to heal itself. Take things one moment at a time and you will get through this! Never give up hope!
Lea P Wright replied on Permalink
As a child and an adult I suffered extreme traumas. Everything you describe points to me suggesting that you look into C P T S D or complex post traumatic stress disorder. I commend you for doing the work you are doing as with time you will benefit from it. I hope that you can get counseling and any treatment available to help you on your path.
Sarah replied on Permalink
Hi! I have so much empathy for you. I am now 45 years old but was also sexually assaulted, physically and emotionally abused as a child by my Father and abandoned twice by both of my parents well into my 20's wherein I continued to get into physically abusive relationships. The PTSD journey is one in which it takes a lifetime to get through. It's so hard for other people to understand if they don't have this disorder. Hang in there, it's a rough journey to recovery but worth taking.
Anonymous replied on Permalink
Wow, sounds like a tough childhood. Let me say I'm very sorry you had to experience any of that. Being young doesn't mean you can't have trauma. Continue to address it. Good luck and God bless.
Anonymous replied on Permalink
Be proud of yourself young man for trying to overcome the abuse that you endured by becoming aware of how the diagnoses you were given affects your life. I hope your healing process is a wonderful journey that brings you peace insight and clarity!!
Nancy replied on Permalink
I am ancient and was secually assaulted three years ago. Fortunately, I have a background in education and I love learning brain information. The big thing I learned is that you can retrain your brain. Just like parents train a child and shape their behavior, you can do the same with your brain. I would wake up panicking at every little noise. But I would talk out loud to my brain. "Good brain. You are alert and protecting me. However it is just the cat (or the neighbor gardening at midnight or the house making a house noise...) Go back to sleep. All is well." I did that enough times, that I kind of woke up one night because the cats were making noise, and caught myself automatically thinking, "Go back to sleep. It is just the cats." I wish you well. As you heal, you will find out that you will be able to recognize and help people who have had similar experiences. No child should ever have to go through what you went through, but much good can come from what was meant for evil.
LS replied on Permalink
What courage and strength you have! It has to work to your advantage more than if you hid and didn't face what happened to you. You are an inspiration to people of all ages that suffer from PTSD! Thank you.
Dswn replied on Permalink
Try EMDR. Look it up on you tube. Helped me alot!! Reconnects the brain.
Anonymous replied on Permalink
It helped me a lot as well, definitely would recommend it! :)
Granville replied on Permalink
I am finding unconcious bias is forming a barrier in actually getting assessed. I have one neurolgist who suspects autoimmune disease and/or Parkinson’s and also knows of fully resolved ptsd 10yrs ago. Ptsd was treated with hospital admission, 26 sessions of EMDR, one to one counselling and cpn/psychiatrist support. No neurological symptoms at time and relates to a car crash. Due to circumstances relating to my son living with me full time had to have assessments etc so he could stop and no evidence of ptsd found.
At same time another neurologist who has not seen me or assessed me knows about ptsd but not the circumstances above and just written it off to functional neurological disorder. It’s a stigma I cannot get rid off but I am fighting the nhs over this.
Anonymous replied on Permalink
I am currently 67, and suffered a traumatic injury in 1958. It wasn't until 2018 that I was diagnosed PTSD and Disassociative Amnesia.
I don't recoil at the instrument of my injury or anything, but I definitely see some kinship in the article!
My decision making "skills" have been sketchy, but the very worst is when I think someone is trying to take advantage of me or pull one over on me.
Jerry replied on Permalink
I'm a 53 year old male who has been Diagnosed with PTSD. Another Month and it will be three years of going through some of the craziest times of my life. I have taken multiple types of RRSI's which I just can't handle the side effects, I have had three stellate ganglion blockers, and EMDI which also did not take like it was supposed to.. So the other Day my Med Manager pretty much told me he has nothing left for him to try so I guess what I'm asking with all of this is if this PTSD has effected the parts of my brain is there anything I can do to fix this issue? Or am I going to have to live with this for the rest of my life? Thanks for your time in reading this and if anyone has that answer I truly would like to know.
Patti replied on Permalink
I'm a licensed clinical social worker and work in a therapy office. I recommend that you find a therapist that does EMDR. It may help you with sorting out the trauma.
Anonymous replied on Permalink
medicine is not always the answer...i have nightmares of screws,nails...any projectile you can imagine being rained down on me after significant other was paralyzed on the job... this is what i call work related stress...one of the first things i learned was that most people go into shock, when for e is was fight or flight..taking the ton of oak boards off of her..but doing the right thing set me deeper into doing wrong things
peter replied on Permalink
You will most likely never read this but learn to become mindful through leaning to look inside..I wish you Peace
Helper replied on Permalink
Stay Strong Sir there’s always hope.
https://med.nyu.edu/departments-institutes/population-health/divisions-s...
Brother Jacob, 42yo replied on Permalink
Kind of an edgy idea for some, but an idea, nonetheless. Perhaps a visit to a place where one can legally and safely have a deeply moving and cleansing, mental and emotional, experience with an appropriately selected plant medicine and a trusted guide. I've heard of life changing experiences from a variety of options. In the U.S., an organization called M.A.P.S. has been approved govt funding for research in treatment of P.T.S.D. with psilocybin and M.D.M.A, for their initial research. They may officially study some of the others, in time. And there are options a plane flight away. A potentially semi-religious level of feeling connected and aided, if carefully used. An idea to consider, when pills aren't helping.
Much love to another member of the human family, and wishing you luck in your journeys,
Jacob
christen bruce replied on Permalink
Please find EMDR therapy- it is with eye movements and reprocessing the experince in the brain
Liam replied on Permalink
In this year the drug used for PTSD
treatment is going to be approved.
That Drug is MDMA. Supposedly in 3 counseling sessions the good majority
of patients recover from PTSD . Look it up on the web and read for your self. And God bless you. Liam
Nancy replied on Permalink
I have heard this. What used to be used for partying will now be covered by your helath insurance!!!
Lisa replied on Permalink
I have been recently diagnosed by a psychiatrist with Chronic PTSD. The first clue that I was dealing with PTSD came over two years ago when I saw a therapist for the first time. At both visits, I was prescribed Zoloft which so far I have resisted to take. My PTSD started from childhood trauma furthered triggered in adulthood from workplace trauma and other heartbreaks that left me feeling unsafe in this world. The worst PTSD symptom that continued to haunt me and caused me continuous distress was non-stop intrusive thoughts. These thoughts would trigger strong emotional reactions internally that I could not shake. It was like I was at times stuck in this loop and the only relief (without medications) was distracting myself by keeping my mind busy with something which would at minimal provide temporary relief at my worst times. Meditating took the edge off but my brain continued in this malfunction way when something triggered it. Less then a week ago, I decided to try acupuncture for the first time. After the first session, I felt immediate relief from my distressing intrusive thoughts and finally felt a calmness to my core and a clear mind. It was amazing. After the 2nd day, slowly I felt some intrusive thoughts come back. After my second acupuncture, these painful intrusive thoughts have fully disappeared leaving me with a sense of internal calmness, peace and a cleared mind. Distressing thoughts and emotions no longer impact me to my core like they used to though I can still feel emotions but now with a sense of balance. My next acupuncture appointment will be my third session in a one week period. For once I feel relief from my symptoms of PTSD and the intrusive thoughts which is my form of flashbacks. Acupuncture is activating my parasympathetic nervous system (the rest/digest system) which is calming my sympathetic nervous system (fight/flight system). I feel so hopeful moving forward that I can manage my PTSDS symptoms and reclaim a sense of quality to my life. If you chose to try acupuncture, do your research and find the right practitioner. For me that has been one rooted in a background or degree in oriental medicine. I wish for relief to all of you suffering from PTSD.
Lynn replied on Permalink
I just wanted to say that I have found great relief with acupuncture, too! It’s been a huge help to me in balancing my nervous system after several traumatic events over the past year and a half. I feel like it’s magic! I hope you have continued on your healing journey.
Lynn replied on Permalink
I just wanted to say that I have found great relief with acupuncture, too! It’s been a huge help to me in balancing my nervous system after several traumatic events over the past year and a half. I feel like it’s magic! I hope you have continued on your healing journey.
Tony Fantasia replied on Permalink
Hello Jerry. I came across your question and, despite the time that has lapsed since you first posted it, I would like to offer my response in hopes that it is helpful in some way. I was diagnosed with PTSD back in 2006 after returning from my second Army deployment to the Middle East as a combat medic (Bagram in 2002 and Mosul in 2004). I struggled with PTSD for many years before I knew or accepted I have it, but it got through eventually. Accepting that you have it is the first step, but even more important is understanding that it is normal and there is nothing "wrong with you". Experiencing trauma comes in many forms and impact each person differently. The first thing that really helped was accepting it and learning to discuss my thoughts and feelings so that they don't get buried and smothered by "what-if" scenarios. Sometimes (most times) the fear and perceptions in my head are 1000% worse than what they are in real life and person-to-person conversations about our feelings are the only way to understand that. My healing accelerated significantly when I took on a hobby (leather craft) and spent time focusing my mind and hands on constructive and creative activities that gave me peace and joy. During this time, I found that my brain was able to relax and process thoughts and feelings on more of a subconscious level. Over time, this helped me accept and resolve a lot of bottled-up emotions about many events (going back to early childhood).
Eventually, I came to understand that I was disassociating from my life and the world by hiding in "fantasy land" and I had lost perspective of my place in "the moment" or the here-and-now. I had to force myself to remain aware of the moment and not drift off to fantasy land by verbally narrating my daily activities to myself. eventually I could do the narration in my head, but the verbal narration kept me focused on the tasks I was performing and kept my mind from drifting. After a while I became more aware of the moments so that, when I came to a decision-making point, I could think back to the moments that lead to it, and was able to make decisions based on a thorough assessment of preceding events, and eliminate chance as much as possible. this resulted in more effective decisions and outcomes and (virtually) eliminated the unfavorable or inconvenient outcomes. This built my confidence and helped me make short-term and long-term goals with less fear of failure and more assurance that I could not just survive on my own but thrive.
I would not say there is ever going to be a cure. It's more like developing a better strategy for managing stress responses by developing a mindfulness and awareness using good coping mechanisms. You will have to deal with this for the rest of your life but, as far as I have seen in my own life, the more you manage it effectively, the faster it becomes an automated process like breathing and blinking. I have been managing my own PTSD for the better part of 17 years now and am feeling stronger and more capable every day. I have lapses and I had to learn to accept them as normal as well. I had to learn to forgive myself for my fallibility and weakness and keep moving forward knowing that my intentions are good and so is my effort. That has to be enough. Anymore expectation than that is a recipe for disappointment.
I am sorry you had to wait a year for a response to your questions, but I hope this offers you some hope and perspective. Sometimes that is all we need. Take care and best wishes in your journey.
E replied on Permalink
Hi this was posted a while ago but I read it without even meaning to and I felt like your pain like it was mine, because it used to be. I went through something similar and my body was rejecting any medication, I felt very stuck and fell into a deeper pit because of it. I know what I’m about to recommend isnt typically socially acceptable but instead of prescribed drugs they try and give us all, I first started smoking weed (which is also actually medically prescribed through a doctor for PTSD not awfully uncommonly). However I then tried LSD which I have done twice now. There are studies on how micro dosing LSD can help with mental illness immensely. I would not take this option/ path without heavy research. But it is worth it more than anything I could explain. You may not go through things you enjoy going through if you fully trip instead of micro dosing, but it never lasts and it is always a necessary trip. Using this form of medicine isn’t something you have to take on the daily. It’s a one time cure all. It’s been three years now and for all three years I have been lifted from the weight of PTSD. Just some food for your thoughts if nothing else
luna replied on Permalink
I am not in the military or have been, but this explained brain injury and PTSD so well and I've endured enough trauma for two lifetimes. My trauma and neglect started at age 4 after my mother died and my dad married a foreign woman by catalog and left us with her in her country. She was nuts and she only hurt me and not my brother. I faced the price of taking my childhood trauma with added abusive relationships the rest of my adult life, then when I thought I was in the clear I spent 13 years locked away from society and suffered psychological abuse by my past husband. For 20 years I was in therapy, had a psychologist for a while, and now am being seen by a renowned psychiatrist. I tried many treatments for PTSD and was hospitalized 7 times for it and have been in outpatient treatment on and off since 2011. I have been on a med I receive as an injection; Invega and finally something that helps, I'm also on the highest dose of Lamotrigine and Lithium, and Adderall to keep me focused on the here and now. I tried EMDR and I got worse, DBT and even though the skills helped after I finished a 2-year stint (once a week), I would relapse. But now my toughest symptom is memory loss for recent things. I do things that either I or someone else notices of which I have no memory of doing or I forget things that don't seem as difficult for others. I started doing some things on my own to treat myself and that is filling my mind with positive memories as a child and young adult, the rest is so horrible there are no finding positive thoughts. As a child, I'll remember laying on a grassy slope watching the clouds and believing my mom is in them, stuff like that. I have very little memory of abuses but do have the emotions and physical scarring. Since therapy, I have bodily aches and pains when I have a repressed trigger with the worst being tremors/shakes. The rage is gone and I'm calmer. I still don't experience true laughter but do giggle on occasion. So, my best reason for settling down is Invega, I really believe this, although I can't help thinking when will the side effects hit? Then I may have to go off of it, or how long will my ins. cover it? It cost more than $1900.00 for each injection once a month! I hope you find the avenues that will work for you before you're much older like me I'm 65.
Anton replied on Permalink
One of the novel therapies for PTSD involve administration of psychoactive substances during therapy. Authors believe that a controlled administration of substances like NMDA allow the client to talk about the darkest corners of their mind and thus allowing to overcome the trauma by facing it head on. I'm only a medical student, but I would recommend you to see a therapist. Drugs that you are given are supposed to reduce the symptoms for you to get therapy, they will not actually fix the root of the problem itself.
Me replied on Permalink
So I suffered long term reoccurring trauma as a child and into my my teen years. Fear so bad that I always felt like I was going to die as that’s maybe because I’ve had my head bashed into walls and physically and sexually and emotionally abused even had a knife held to my throat by my own mother telling me she was going to kill me because I wanted butter on my toast. I’m 34 now doing ok but let me tell you I’ve been through therapy with countless different types of them and the drugs they’ve had me on were such high doses it actually created its own physical health problems with me which were counter productive. I’ve self medicated with these drugs and Then some at both high and low doses. From personal experience with lsd in high doses(only because I had gel tabs and you can’t really alter the dose) .. well let’s just say I saw the universe below me and had outer body experiences.. I can say for a short time until my next trip that I found new appreciation for life itself and I wasn’t so angry or afraid but after a while that wore off. Mushrooms on the other hand in small doses were amazing... I laughed so hard and just was able to be free and live like My past didn’t exist and I wasn’t scared of things like I normally would of been or reacted crazy like I have in the past because I felt threatened in such a small way. In high doses (like eating an eighth) I would melt into myself and found the darkest corners o didn’t want to be at. I even became Cheshire the cat with only my head floating.. MDMA was great tried it twice but the hangover was miserable. It was like I had all my happiness sucked out of me again. Salvia was interesting but more paralyzing for 20 seconds or so.. DMT now that’s another world.. it was like living as I was glass breaking through dimensions all the while everything around me was like a kaleidoscope. Only took one hit lasted for a minute or so. I think mushrooms and lsd in very very low doses as a prescription would do more good than any of the others I’ve had experience with. I wish there were more studies on those. I know it is in some state but it’s only for terminally ill patients. Which is unfortunate because it could do some great healing with proper dose and a good Psychologist... not a therapist or a special hypnosis one (that crap doesn’t work) Psychiatrists just give you meds and don’t really help you through anything.. . the only person who has ever slightly helped me was a psychologist.. some great people there, they are just so extremely expensive! Wish I had the capacity to go to school for it. Studying is hard with Ptsd.. it’s even harder to hold a job to afford good treatment and function “normal” in society. It just sucks
Willow replied on Permalink
I personally suffer from PTSD. What I found most helpful was therapy. It's very painful and difficult at first but a necessary step for me personally. I took medication to supplement the therapy and make living day to day easier. The mood stabilizer Lamotrigine was very helpful to me. Therapy and mood stabilizers didn't fix everything, but I learned coping skills that have helped me survive flashbacks, anxiety, and depression. You aren't alone, brother. Hang in there.
Anonymous replied on Permalink
It would be really helpful to know the author of this piece but I couldn't find one listed anywhere
Anonymous replied on Permalink
If any is looking for the author they credited it in the gray box above the comments section. It was ripped straight from that website. Hope this helps :)
Alicia W replied on Permalink
I am not a service member, nor a retired veteran but this article has helped me understand a bit more of why I may have inappropriate fear responses to places like waiting rooms. My therapist explained to me that my “trauma brain” may react to generally benign situations. Thanks for elaborating a bit more for me.
Warren replied on Permalink
I'm glad to see another non-service member here, especially someone who can relate. I too got some good insights.