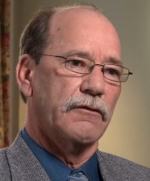
Ron Broughton of Brookhaven Hospital talks about ways that healthcare providers can use flexibility to help their patients continue to make progress on a daily basis.
Posted on BrainLine November 7, 2012. Reviewed December 25, 2017.
Produced by Victoria Tilney McDonough and Erica Queen, BrainLine, and Dan Edblom.
About the author: Ron Broughton, MEd, LPC, CBIST
Ron Broughton, MEd, LPC,CBIST is the chief clinical officer at Brookhaven Hospital as well as chairman of the Ethics and Performance Improvement Committees.