At Rush’s Road Home Program, providers use evidence-based cognitive processing therapies and other data-driven therapies like mindfulness to treat veterans with post-traumatic stress disorder (PTSD). This intensive treatment model effects far more cures for PTSD in veterans than the traditional, one-on-one, long-term psychotherapy model. Rush is working to offer their therapy model to other populations who may experience PTSD like police, firefighters, first responders, and emergency department staff.
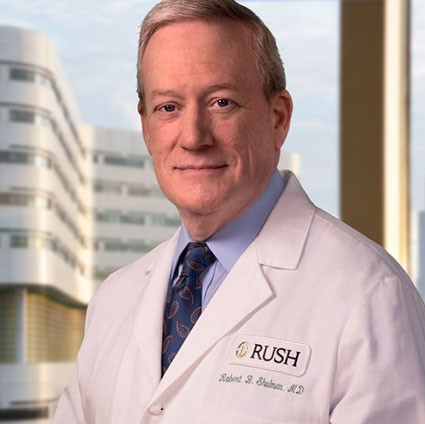
Robert Shulman, MD is the director of the Road Home Program at Rush University Medical Center, part of the Wounded Warrior Project's Warrior Care Network.
For information about treatments for PTSD please visit The Treatment Hub.
One of the things that the Road Home program does really well is that we use certain evidence-based therapies, cognitive processing therapy and other cognitive therapies that has evidence to support its use as a direct intensive treatment for the symptoms of PTSD. Our response rates are tremendous. We can affect cures in some individuals, people who after their intensive treatment with Rush, no longer exhibit symptoms of PTSD, on rating scales, and we follow-up six, twelve months out and they have maintained responses. It’s a lot more efficient than the older, more traditional model of weekly psychotherapy where you sort of talk about things and such. That stuff just doesn’t work with veterans. You got to get focused and work through it. And so, it’s a very structured kind of therapy that becomes intensive. And with it we incorporate other evidence-based therapies, including mindfulness. Mindfulness may sound a little hokey, but it actually isn’t. If you look at the physiological changes that one has when one is in a meditative state, the predominant brain wave is an alpha wave, that is the resting regenerative state. We’re actually helping put the brain into a healthy resting state such as people who mediate, by practicing mindfulness and that has healing benefits for the brain. When you’re talking about circuits that have been disrupted, provides healing to us. So that, along with cognitive based therapies, that have been proven to be very effective. Our hope is that the work that we do will translate to other populations who suffer PTSD, not just military. We have discussed treatment to first responders, police, fire, and other emergency workers. At the start of the pandemic, we were actually working at screening our own hospital staff for symptoms, and we were ready to initiate our therapies for our own staff that were experiencing the trauma of working on high stress COVID units in the emergency departments. We hope that what we learn working with veterans will translate one, to other treatment centers picking up these techniques and using them. The Veterans Administration is now working towards developing more structured programs for PTSD rather than the older, inefficient one-to-one ongoing lifelong therapies, and we hope that our work will translate to treating other populations as well. BrainLine is powered in part by Wounded Warrior Project to honor and empower post-9/11 injured service members, veterans, and their families.
About the author: Robert B. Shulman, MD
Robert Shulman, MD is the Director of Road Home Program and currently acting chair of the Department of Psychiatry and Behavioral Sciences at Rush University Medical Center and Mental Health Service Line Director for the Rush University System for Health. He is a graduate of Lewis & Clark College and The Chicago Medical School (with many clinical rotations at the VA Hospital).