Chutes and Ladders
After every full- blown crisis comes the moment when the adrenaline retreats and the shoulders sag. The person is out of the critical zone. The patient has been discharged from the hospital. The divorce papers are signed. The father has been buried. The chemo has started. This is the moment when the real work begins. This is the “ever after” part — the new life, post- crisis, that cries out for definition. There are absolutely no shortcuts through sorrow and pain or to mitigating the day- to- day terror of a crisis. There’s no going around it. It’s like a long, dark train tunnel in the Alps. All you can do is go straight through it. Buckle your seat belt, pray, do your homework, stretch, keep breathing, turn to literature, gather collective wisdom for solace, brace yourself, talk it through, hold on. Grief, loss, and the twisting roller coaster of emotions that accompany it are all about endurance. Sheer endurance. In my own crisis, this new period began the moment my husband was out of the acute- care stage. Bob had woken up from the coma, but he barely resembled himself. His brain was missing words and names, and he was having trouble tracking conversations. He couldn’t say “Tony Blair,” but he could pronounce “Mahmoud Ahmadinejad.” Each day brought new accomplishments and new worries. He was still very much a patient and not yet back to being a husband and father.
By nature I’m largely a happy, positive person. But in the wake of Bob’s injury, I’d been felled by a pretty large ax. There were days when I thought it would be better just to lie down and sleep for a thousand years. Other days I wanted to sell my kids on eBay to a mom who would be more loving and attentive. There were many mornings when I couldn’t wait for bed, when I didn’t get outside once, when my thoughts and fears fluttered futilely against the side of my brain like bats trapped in a loft.
But I wouldn’t allow myself to give in completely to those feelings. For two long months in the hospital I remained up, dealing with doctors, decisions, my four kids, Bob’s whole family. Even after Bob awoke from his coma, I approached his care and my relationship with him like a chirpy Doris Day: determined not to let him falter, guarding against his sadness, constantly pumping him up like a manager encouraging a prizefighter from the corner of the ring. Part of my job was to point out improvements, like a scientist studying tiny molecular changes under a microscope.
In particular, I knew, I had to stay positive for the children. Observant twelve-year-old Cathryn, especially, watched my every move. She examined each facial expression and lurked behind corners when I was talking to other adults on the phone. Earlier, during Bob’s coma, she even listened in on the call when the neuropsychologist from the hos•pital was talking to me candidly about the likelihood that we might need to park Bob in a nursing home. She was suspicious and terrified.
Which meant that it was that much more important for me never to let down my guard. But for all my natural optimism, the pressure to stay positive was just a little too much, and as soon as Bob was safely on the road to recovery, I knew I was bound to crash. Every time I rocketed down, I struggled back up; if I’d been up too long, I knew the bad days were destined to inch back. Up and down, up and down my emotions traveled, as if they were playing a game of Chutes and Ladders.
Still, by the time Bob had begun the daily, rigorous schedule of therapy, I knew I was hitting rock bottom. The bad days far outnumbered the good, and I felt like I was in free fall. I would wake up in the middle of the night with all of my deepest terrors flying at me like birds, dive- bombing me with their beaks, and I was helpless to shoo these anxiety attacks away.
When I did manage to fall back asleep on those nights, the sleep was usually fitful. In the morning I would lie there leaden, sodden, and have to force my feet onto the bedroom floor, while Bob snored gently next to me with part of his skull missing, needing every minute of sleep for his brain to keep healing.
Those early moments of the dawn used to be my coveted hours, a time filled with the rich possibility of the day. Instead, I now felt our life as a family cinched tight as a belt, circumscribed by Bob’s injury.
Those mornings, I barely held it together while I got the kids dressed and off to school and then my husband out the door to his daily rehabilitation therapy. Finally, one morning when they had all gone, I just collapsed, fell onto the couch sobbing in the quiet hush of my home. These were gut- wrenching, back- heaving sobs. I was crying out the whole last few months and tasting the fear of the unknowable coming years.
It was clear now that, after surviving everything else, I had finally hit my wall. For so long, I had been in “go” mode, always moving forward, making decisions. Like an Olympic athlete facing the toughest race of her life, I had cleansed my body of alcohol, soda, coffee, anything that might dull my senses or distort my mood. I was careful to keep all of the practical parts of me alert, but I had not allowed myself to grieve, or to feel from my nerve endings. And now here I was, back home and with the luxury of time, since the immediate needs of Bob’s physical injuries had been handled. The levee was now crumbling.
That morning of my complete despair, my friend Alicia stopped by. She was deeply worried by the new rag- doll me she found on the couch, and as I talked through my darkest fears, I began a spate of fresh tears. What would our life be like? What if his progress just stopped? What if the man who so loved his job, who had functioned as a kind of quarterback, became instead a useless extremity, something resembling more of a mascot than a team player? And the most horrifying question: What if I didn’t love him as much in the end? What if my love for him slowly eroded, little by little, if he remained diminished? “I need some help,” I croaked. “I need professional help.”
“And you may need medication,” she said. “In your place I might need medication too.”
“Maybe.” I nodded, but my one encounter with Xanax, immediately following Bob’s injury, had been a disaster. The pill had made me feel dull, useless, and not myself. I’d never liked that out-of-body experience and I didn’t want to consider going through that again. I would have been a dismal groupie at a Grateful Dead concert.
After Alicia left that morning, I resumed crying again. And then the oddest thing happened. I closed my eyes and suddenly, a soft, white light blossomed, a burst of enveloping warmth, indescribable but somehow calming. Mysteriously, a feeling washed over me that hushed me, told me I would be okay, this would all eventually be all right. There were no flowing robes and no golden staffs. It was more like an authoritative voice. It was bigger than me, more than me — that’s the only way I can describe it now. And in that moment, the terror subsided as quickly as it had consumed me. Once again, I had gone steeply down a precipice and crept back up.
Still, I knew I could trust the light I saw and felt that day on the couch. The mere existence, the possibility of that kind of calm, gave me hope. I didn’t need medication, didn’t need to numb my mind in order to survive, I thought. Someday I would move through this. As awful as I felt right then, there would have to be better times. Life simply moves on. People adapt, or so I told myself.
Around that time, another sign came to me. This one shook me deeply but ended up giving me strength: my diamond ring broke. When we had lost a child years ago, Bob had given me a small band of seven diamonds, one for every year of our marriage. It had been my idea to remember the child we’d never known and honor the years of our union. All of a sudden, as I was driving to our friends the Bakers’ house, it simply snapped. Fingering the roughness of the cracked metal, I looked down in surprise to see the ring intact, but split across the band. I froze at the implied symbolism of this sudden, spontaneous break.
Panicking, I pulled Susan aside as soon as the twins were playing upstairs. “This ring was for us, for Bob and me,” I said. “It’s broken — does that mean that Bob is broken? Why this timing? Why now?” I needed to understand how this could possibly not augur an ill outcome.
Susan looked at me coolly. “Don’t you see, Lee?” she said without hesitating, in her southern comfort accent. “This is actually a good sign. Yes, Bob is hurt, but your marriage is intact. The ring didn’t fall off. It’s still a circle, and you didn’t even lose a stone. It is a symbol, Lee. Bob is going to need to be fixed, he is broken, but it’s all still there inside of him.”
I will always love her for that interpretation, her soothsaying. Susan had talked me down from the ledge. But my connection to future hap•piness was so tenuous, so unknowable, that I needed to spread my faith out to encompass everything — to, in effect, hedge my bets. I needed prayers and chants and symbols and omens and objects to keep myself up, to keep myself going. In point of fact, I needed all of the goodness of the universe on my side to pull us through.
While Bob was as fragile as an egg on a spoon in a children’s relay game, I hung on everyone’s encouraging words. I was the eager, crippled woman in a religious revival tent, riven with sorrow and praying for a miracle. My friends and family, the therapists and doctors, our minister, all of these people were the shamans of my tribe. Although I knew they did not work magic, I desperately wanted to believe they could.
Take care of yourself, everyone said. Make time for yourself, consider what your body needs. But it was impossible. If they could have seen my life, the overwhelming crush of responsibility mixed with all of the little things, the permission slips and school notices, the tax extension and the haircut for Mack, they would have known better than to utter those words. How does any caregiver really make time for herself in the midst of a cyclone? I just hung tight to my game of Chutes and Ladders and waited for the end of the ride.
The months ticked on, and soon Bob was approaching the date for his surgery to place the acrylic skull over his exposed brain. He had lived with a plastic climbing helmet on his head anytime he was on his feet. It would be a long and involved procedure and not without risk. Essentially, they would have to peel back Bob’s scalp and lay it over his face as they fine-tuned the size of the acrylic skull plate so that it would fit as precisely as a puzzle piece, then set it into place and use a special epoxy to bond it to his existing skull bone.
He was understandably frightened and anxious. Unlike the dozens of surgeries he had undergone when he was unconscious, he was well aware of this one and its risks. And the thought of having neurosurgery terrified him.
With all of this pressure and worry building up, and everyone still reminding me to take care of myself, I decided I was finally ready to talk to someone. After choosing a therapist near my home, I went for a few sessions. Each time I found myself crying for a solid hour, asking the woman questions she couldn’t possibly answer about Bob’s ultimate outcome and what would become of us. It soon became clear that my abstract whining in the psychiatrist’s office wasn’t getting me anywhere solid. She helped me develop some imagery — I was to picture myself on a raft in the middle of my favorite lake — but the night terrors still stole into my room each evening and capsized my calm water scene.
I liked this therapist, I really did, but I found the whole idea of grief counseling disturbing in that, no matter what I was doing or how I was feeling, if it was nine-thirty on Wednesday I had to drop everything and go prepare to grieve. Even if I’d been having a good day, I had to be ready to leave that room after an hour with tissues pressed to my nose, sniffling or holding back sobs. It felt like mourning on cue, and I grew to resent it.
“You need body armor,” Dr. Mary Hibbard announced to me one afternoon. Although she was Bob’s neuropsychologist in New York, she had agreed to counsel me too. She knew Bob; she monitored and marked his progress. She had concrete answers about brain injuries and examples of other success stories, though admittedly they were few and far between.
“I need more than armor,” I told her glumly. “I need an armed personnel carrier.” Her suggestion sounded like a nice little euphemism for popping some mood- altering pills. For months I had resisted the idea of an antidepressant, believing that I could find my own equilibrium. Yet something in what she said struck a chord for me. Here I was in a doctor’s office sobbing, terrified — I didn’t sound so levelheaded at all. And here was a wise woman I respected giving me a practical solution for how to take care of myself, one that didn’t require siphoning resources from anyone who needed me. Finally, at that moment, it seemed like a sound rationale. Maybe it was time to seriously consider medication. I was in emotional pain, as one doctor would explain to me months later. And emotional pain is just as real and uncomfortable as the physical kind.
So I agreed to try an antidepressant, since if nothing else it would allow me more peace at night, more sleep, relief from the now-familiar anxiety attacks that seemed to find me as regularly as a Swiss watch.
As it turned out, the Paxil was actually a help. It didn’t make me feel like a rodeo clown, or like skipping across four lanes of traffic in a convertible. I didn’t have to suppress the desire to sing “The Battle Hymn of the Republic” at the top of my lungs in the shower.
It just made me feel, at last, like me. It resuscitated the old Lee. It created a trampoline under my free fall, a barrier that allowed me to stop myself when I became anxious so that I did not go any lower. It was all very subtle, but over time I began to notice that the fear was more muted and my ability to feel some joy was restored. The anxiety had been driven back down into a containable place where I could talk and reason with myself, using my inner voice. In short, the medication had allowed me to recognize the emerging outlines of the old me.
That prescription eased me through Bob’s operation — which was successful — and beyond. And as Bob healed and returned more and more to himself, so did I, although I didn’t spend time thinking about the medication.
“Are you still taking those pills?” Bob would ask me periodically, months after that last big surgery, when he was back at work and life seemed finally to be moving in a fairly straight line, with only occasional kinks of uncertainty on my part.
“Yup,” I’d answer.
“Why?” he’d respond quizzically. “Aren’t we all doing well?” And we were. But if Bob had any little setback — a tired day, a confused moment — if there was any tiny wrinkle that only the expert eye of a wife would see (and I saw everything), it might throw me.
I wanted to take the antidepressants a little longer, I told him. I’d know when it was time to stop, I said. But the truth was, I still wasn’t sure. What if now I needed the medication in order to be “my old self”?
I didn’t like the idea of taking these pills indefinitely. Not only did they make me sleep a lot more, but I wanted to see what I would be like now that life had calmed down. I wanted to kick out the crutch and see what Lee looked like in the aftermath of a crisis. It would be Lee raw, Lee without the lift.
Could I still have a bad day and then simply recover? Would I be able to go to bed and tell myself that tomorrow would be an improvement — and then really make it better? I wanted to know.
In the past, I had always had the power to talk myself out of a funk, the way I would buck up other people. I reasoned with myself through bad times and focused on the fact that often good things really were just around the corner, like the moment of peace and light on the couch that one morning, or the hopeful interpretation of the broken ring. I had once had a fairly dependable ability to almost will myself happier by focusing on the small acts that lifted my spirits: an outing to the movies with a friend, a brisk walk down by the nature sanctuary in our town, spoonfuls of raw cookie dough. Would I still be able to do that in the aftermath of a crisis, would I still be able to glimpse a little light at the end of every tunnel? Or had the process deformed and mutated me? How could I tell?
And so one day I simply stopped. I didn’t say anything to anybody, but I just stopped taking the pills. I didn’t flush them down the toilet or do anything dramatic. I just stopped. In hindsight, I probably should have consulted my doctor first, but I felt certain I knew best what my body and mind needed.
So far, so good, I decided after a while.
Of course I had days here and there where I was down, but they were usually followed by days where I was relatively happy again. I found joy in a cobalt- blue sky, in going for a swim or a walk with a girlfriend. In short, my motor still worked. I still controlled the gearshift, and I still knew how to pull myself out of a tailspin. This was good. This was better than good.
And when a lowish day came by, or something seemed difficult, I talked to myself. I felt for the trampoline floor with my toes, and it was still there. It was not artificial; it had not been medication- induced. I had wanted to know that not only could we survive a crisis but that my former set point for happiness could rebound too. And for the most part, it had.
In my life, what the big miracle of Bob’s recovery did more than anything was to widen the aperture inside of me to witness the presence of small everyday blessings. The big moments are easy to spot. But the real challenge, the art form, is to find gratitude in much simpler things. We need to be open to feeling the power of a life made up of many little shards of white- light experiences. These moments of grace, as I think of them, are as real and as powerful as the headliners. They help us to throttle up, to rescue ourselves from a nosedive, as surely as those little white pills did for a while for me.
I see these little blessings in the gift of a friend’s healthy newborn baby, a clean mammogram, or the really, truly satisfying snatches of conversation I have with my father now, when he is having a good day and can clearly remember the parts of his life. People talk a lot about living in the moment, but to do that, to really achieve that, is to be able to fully participate in all the unarticulated goodness that makes up our lives. And of course, that kind of focus isn’t possible every single day. But I try now to give it all my attention when I tiptoe into my children’s bedrooms in the morning and stroke their hair as I wake them for school. I count my blessings for having sisters and girlfriends with whom I can unburden and be as comfortable with as a second skin. It is one of life’s small gifts to be able to ease someone’s pain, to hold their fears for an hour or a day. It is truly miraculous to sit and watch the sun rise and set, or to study the perfection of a colorful spring blossom.
In the second summer after Bob’s injury, I could finally say our lives felt secure. It had been eighteen months since our world, like Dorothy’s farmhouse, had been rocked off its foundations and gently set down somewhere else. We were not in Kansas anymore. But we were in firmer territory in some ways. We knew the fragility of life firsthand — we lived more in the present; I believe we all did. I was aware of the passage of days and weeks, aware of how finite the time was that I got to be a mom and enjoy my kids on this earth before they became full-sized human beings with independent lives.
None of us would ever choose to rupture the veil of innocence that shelters our children. As a parent I would have liked to spare them from the worst of it, but that’s ultimately not realistic. You cannot protect them all of the way. That’s not how life works. And that’s okay. But in the grateful aftermath of our family’s collective sorrow, I tell myself that my kids have learned more from the difficulties and hardships they have witnessed and endured than they ever would have otherwise.
The routes my children constructed to navigate around the fear and loss surrounding their father’s injury have forged their capacity to truly engage in their own lives, to be empathetic and to genuinely care for others. I have no doubt that they can already handle situations far beyond what many of their peers can. They have built up the same capacity that now sustains me, the ability to roll down with the chutes and up with the ladders, to reorient themselves and search for hope in even the most terrifying situations.
This fall I was pulling out of my driveway, distracted by the twins, who were not buckling their seat belts fast enough. Nosing into the driveway with spectacularly bad timing was our letter carrier in her boxy white truck. Looking left when I should have been looking right, I suddenly slammed into the truck’s side with our brand-spanking-new SUV.
After I made sure the girls were all right I hopped out, mad at myself. The mailwoman was already out of the car, shaking with fear and worried, I’m sure, that Suburban Soccer Mom would start screaming at her. A small wiry woman, she was jumping from foot to foot and swearing as she pulled a pack of cigarettes out of her breast pocket and lit one.
“It’s my fault,” I said, worried by how distraught she looked. She was already calling her supervisor as we circled around her vehicle. Her old battle-ax of a truck seemed to have suffered only one fresh scrape on the bumper, but my SUV was completely bashed in on the right back side. One of my girls picked up the shattered red taillight housing and handed it to me.
“Damn,” the mailwoman said under her breath, shaking her head and taking a deep drag of the cigarette. “My supervisor says he’s gonna have to come out.”
“Don’t worry,” I said, calmly. “I’m not upset. Everybody is safe. It’s just a car.” She didn’t look completely convinced. “You can’t ruffle me anymore,” I said, and I flashed her a smile and reached for humor to calm and reassure her. “My husband was blown up by a bomb. Now, that’s something to get upset about.”
“What?” she responded, with a physical jolt. “My God ...is...is he dead?”
“No, no,” I assured her, “he’s fine now. But it makes things like busted cars not that important in the big picture.”
“Look at this,” the mailwoman said abruptly, lifting her shirt to show me a road map of scars crossing her abdomen and chest.
“Wow.” I whistled softly. “What happened?”
“When I was five I fell out of a window and survived. And later I got breast cancer.” She gave me a winsome smile, one gold tooth glinting toward the back, and then she took another tug at her cigarette.
“Man!” I said, looking her right in the eyes. “Ain’t life a bitch!” And then, right there on the driveway with the broken red plastic taillight, we both just started to laugh.
What I know Now
When bad things happen, we all dream of rewinding the tape. Every one of us would go back to the minute before the car skidded off the road, would make the appointment for the colonoscopy a year earlier, would stop ourselves from turning our backs for a second as our child was swimming or when the ladder holding Dad started to wobble. But we can’t, and so we do the only thing we can: we take those bad things and turn them into situations we can learn from. It’s human nature to try to pan for gold, to find a positive slant in something so negative, because anything less would feel like defeat. Euphemistically, these tragedies are called “life experiences,” but for better or worse, they are some of our most powerful moments. Thankfully, my own family has come out the other side of our own crisis. First, we survived; then we slowly learned to thrive again. And in the process I have been taught some important lessons about being a caregiver, mother, wife, healer, friend, motivator, and the grateful recipient of oodles of love, goodwill, community support, and prayers.
I am frequently approached by people who have been through very difficult experiences with their loved ones, and after sharing their stories, they are quick to minimize what they have endured in relation to my journey. “But my mother’s cancer was nothing like what you went through,” they offer. And I disagree. I say that all of this collective suffering exists on the same frequency of human emotion. Grief is not a competition. Sorrow is sorrow and fear is fear and loss is loss and we humans are all traveling on the same bandwidth in life.
In the past year, since the book I wrote with my husband, In an Instant, was released, I have traveled around the country and met many people and families who have suffered or are suffering. They have journeyed along what I call the grittier pavement of life.
When I relate what I have learned through tragedy and recovery, I see a lot of heads nod. People want to talk about what works for them and what those who have not walked in their shoes should know.
I have often been asked to share these lessons. Therefore, drawing from my own experiences and what others have told me, I have created a list of things to consider if someone you know or love is facing a life-changing trauma. The following tips, while not necessarily novel, seem to have a universal appeal — perhaps because the big moments, the teaching moments in life, are often a series of unplanned, sometimes catastrophic events with no rational explanation. Because, yes, bad things do happen to good people.
1. DON’T HANG BACK — MAKE CONTACT
Though I would venture to say that just about everyone knows someone who has had to face a personal disaster, most people who haven’t experienced a tragedy or serious illness at close range have no concrete idea of how best to approach the person who is suffering. They don’t know exactly what to say or what to do. Everyone wants to get it just right, but it’s frequently hard to gauge what is appropriate.
Coupled with that uncertainty are also very basic, human reactions when someone is sick or injured. Another’s accident or illness often seems to threaten our own lives, reminding us of all the frightening possibilities that could befall our family or loved ones. Sometimes these emotions can be paralyzing. But it is crucial not to hang back: the bravest and most wonderful thing you can do is to be there for someone else, even if this takes you completely out of your comfort zone.
When something goes wrong in a friend’s life, it is essential to acknowledge what is happening. Call people or reach out when you learn they are ill or going through a difficult time. Don’t give up on them if they try at first to push you away, but take your cue from them. If your own emotions won’t allow you to engage the person without making them uncomfortable, step back and write a heartfelt note instead. In either case, do come back — they will need you later on. Make sure they know you love them and care about them. We all need comfort and companionship. We just may need it at different times and in different doses during the journey.
When Bob was injured, I was surprised by some of the people who stepped into the void in amazing ways to help. In many cases they weren’t necessarily the people I had expected. People react to misfortune and mishap in very different ways.
For the people in the vortex of the crisis: it’s important to keep in mind that just because some folks don’t raise their hands to help doesn’t mean they don’t care. An inability to cope with what you are going through could simply mean that friends and acquaintances are nervous or anxious about how best to approach you and tackle the situation.
2. HELP THEM FEEL “NORMAL”
When I was living in a hotel room in Bethesda, with Bob in his coma, one of the many fabulous gifts of help came from my friend Kitty, who lived in D.C. We were trying to convert family videos to DVD format to play in Bob’s room so that he could hear his children’s voices, but we were having trouble. Kitty just showed up, took the tapes, and didn’t ask pointed questions or demand information about Bob’s condition. She never expected to see Bob in the ICU or to get any inside scoop. She told me about her kids and her husband. She entertained me with stories about her workplace. She just came and helped. Two days later the tapes arrived at the hotel desk, all transferred onto DVDs so we could play them for Bob and help his brain knit itself back together.
My friend Colleen sent me a certificate for a massage, which I ultimately used even though I worried about Bob the whole time. Rebecca came to my hotel suite and quietly filled the fridge with healthful food, arranged flowers near the bed, and organized and prioritized all the mail that had been forwarded. She never asked me one prying question about Bob’s condition or prognosis. Instead, she waited until I was ready to talk.
These simple, calming acts and my friends’ way of treating me as “normal” were exactly the tonic I needed. In the midst of the tornado raging around my family, I loved it when people talked to me about their aging parents or the fact that their child needed glasses. My world was so unimaginable, I had lost the language of reciprocity. Sometimes when a person’s life has changed so much, they want to hear what normal sounds like; they want you to treat them as if their world is just like it used to be.
3. RECOGNIZE THE POWER OF HUMAN TOUCH
When you are visiting the person going through a difficult time, treat him or her like a human being — not a patient. Especially with children, get down on their level and look them right in the eyes.
Don’t be afraid to make physical contact. Most illnesses and injuries are not contagious. Touches and hugs are one of the most healing things one person can do for another. Everybody wants to feel like a human being. A loss, illness, or injury gives people a sense of being exiled from the herd, so do whatever you can to make that person comfortable — overlook the tubes and machines they may be hooked up to and just focus on that loved one or friend as an individual.
I remember when Bob and I visited Jose, a young marine with a severe brain injury, in Bethesda Naval Hospital. Since Jose’s arms and wrists were still raw with wounds and crisscrossed with tubes, I chose to focus on his feet. I rubbed them as I talked to him, wanting just to give him that basic physical human contact. Jose’s mother and sister said that they could see him relax instantly, because someone was treating him like a person and not a patient. Simple acts can go a long way toward restoring dignity to a human being.
4. ESTABLISH A HEALTHY INFORMATION EXCHANGE
This means three things: not demanding information from a patient or caregiver; sharing information that may help a patient or caregiver; and knowing what to keep to yourself.
In moments of crisis, everyone wants information, and many people deserve to get it from the source, since lines of communication can be confusing and not knowing can be terrifying. Luckily, the Internet has made it much, much easier to disseminate information and update family and friends. There are incredibly helpful websites devoted to caring for someone, such as CarePages and CaringBridge, which act as a lifeline for friends and loved ones during times of crisis. A person can post messages about their own condition or their loved one’s progress on a Web page for others to read. These sites also offer a place where people can write messages of encouragement to a patient, so that he or she can check in when it is convenient. This ensures that the individuals in the crisis don’t have to spend precious energy reaching out to everyone, returning phone calls, or even sending mass emails.
When you’re visiting someone going through a difficult time, don’t ask questions that make them recount the whole ordeal, the facts and statistics, or the road ahead. They may not want to talk about the issue at all. Just take their lead when it comes to conversation. Resist the urge to share your own stories about similar illnesses or diseases and other people you know. Many people think that comparisons are comforting or hopeful, but these stories can actually be terrifying or even insulting. More general encouraging comments or expressions of sup-port — such as “I know how hard this is because I watched my mother struggle with cancer” — may be a better way to let the person know that you understand some of what they are going through.
Also, this is not the best time to try to rekindle a two-way friendship that has been a “Christmas card” relationship for years. If you want to let a person know you are there for them, a newsy written note or email with no requirement for a reply is a wonderful gift. It can be digested when the time is right. I loved reading through cards and notes before bed, since it made me feel connected to and comforted by the people who were caring about, and praying for, me and my family.
Some of the biggest gifts were the “Bob stories” people shared with me in their notes and letters. I read about humorous or kind moments people remembered, some I had never before heard about. As with those who have lost a loved one, I cherished these letters over those with general expressions of sympathy because they brought me closer to Bob at a time when he wasn’t present.
Ultimately, the best thing you can do is to simply listen to the person you wish to comfort. Be sure to let them know you are there whenever they need to talk, anytime. You don’t always have to have a solution or good advice; sometimes people just need to unburden themselves, or simply say things out loud.
5. AVOID OVERMOTHERING
Certain physiological things happen as a result of stress or grief. The normal circuits in the body are altered; adrenaline floods the physical plant, and the endocrine, circulatory, and digestive systems may go through drastic physical changes. The caregiver, as well as the patient, is damaged, in crisis, and sometimes things inside their brains don’t work the way they normally would.
Do not repeatedly tell the caregiver to eat or sleep. They cannot. They are operating on adrenaline, especially in the early stages. Food is only fuel, and sleep is hard to come by. And don’t try too hard to pry the caregiver away from the patient’s bedside for a bite or a walk around the block. They may not ever want to leave their loved one’s side, and that’s just fine. But also remember that if they say they don’t need help with anything, they do. Don’t be afraid to take charge in nonthreatening ways to ease their daily burdens.
While I was camped out during Bob’s stay in the ICU, my friend Lauren knew that I liked decaf lattes, sushi, brownies, and the special corn and crab soup from the hotel room service. In the early days of our own crisis, I would return from the hospital, shattered and in shock, and find these items waiting for me. She didn’t nag me to eat or urge me to care for myself; she just took care of me quietly, because she knew I wasn’t thinking about food.
Often someone will be designated the point person for the family in crisis. They may be in charge of scheduling meals to be brought in or helping with rides for kids. That person will most likely have a good handle on what needs to be done and what the particulars are. Work through that person and respect that channel of communication, especially initially, no matter how close you are to the individual going through the trauma. That point person is there as an important buffer, to spare the rest of the family or the patient from the unnecessary details.
There are wonderful websites like carecalendar.com, foodtidings.com, and livestrong.lotsahelpinghands.com that allow people to sign up to deliver meals or to help with care for others. For the caregiver, this makes the job of assembling a network easier; volunteers can log on at home and participate as needed. And for caregivers and family members of the ill or injured, there are now informational Websites that can help empower them with useful tools that can be downloaded. Partnersagainstpain.com, for example, provides printable templates for pain diaries and medication schedules to help caregivers stay organized. If you are not a family member or close personal friend, helping from a respectful distance, at least initially, is often the best course of action.
6. BE SENSITIVE TO WHAT THEY NEED TO HEAR
Don’t be afraid to acknowledge the person’s pain. It’s okay to say “This stinks, but I’m here every step of the way.” The most helpful comments you can make involve letting the patient or friend know they’re being heard.
This is a delicate balance because you don’t want to minimize things with trite greeting-card philosophy, but nor do you want to underscore the dire nature of the person’s situation. This is where you need to use your sixth sense and assess where that person is, emotionally, at any given moment. It may seesaw from hour to hour. Take your lead from them about what you think they need to hear. It’s always comforting to be told, “Let’s talk about you for a moment — I’m here to listen if you feel like unburdening.”
One of my most precious e- mails at the time came from our friend Jim Wooten, a colleague of Bob’s at ABC News and a veteran reporter and writer. It arrived at a time when I was tired of hearing about how incredibly strong I was but, rather, just needed to hear that I could simply do this. That it was all possible. Jim wrote,
My only counsel to you is this: make sure to take as meticulously good care of every aspect of your beautiful self — physically, emotionally, and psychologically—as you do of Bob and the children. I can’t stress too much how important that is for both the short and long term, and for everyone involved. You must already understand that you are the most critical component in this difficult equation; and without you as a vibrantly healthy person, it gets even more difficult...and, dare I say it, maybe impossible.
I told you in the hospital that my mother-in- law had a motto about her own life, with all its ups and downs: You play the cards you’re dealt. I realize in retrospect that it was a fairly silly and perhaps a slightly cruel thing to say to you, especially given the awful cards you’ve been dealt in the last three months. It’s possible that the best approach really is to never stop trying to get your hands on the deck and start dealing them yourself. In other words, to begin determining, to the degree possible, your own destiny and direction.... It seems to me that the more you’re in control, the less disappointed you’ll be in what goes on.
I printed that email out, and it still makes me cry when I read it and sense the kindness, empathy, and honesty embedded in the message, the stark and simple concern for me above all else at that moment. I taped the email to the window over my computer at home and vowed I would never stop trying to get my hands on the deck. And somewhere, in that grueling process, I would try to set an example for my children in the midst of this frightening tailspin.
7. THINK PRACTICALLY ABOUT WHAT PEOPLE REALLY NEED
Food, in any time of crisis, is one of the most useful gifts. People have to eat if they want to keep going. This is also true in a hospital setting, since it can be used to “gently bribe” the nursing staff and win friends among the medical professionals. A batch of brownies works wonders at improving the speed with which a call to the nursing staff is answered. The “Brownie Lady” in room 205 also has a much better chance of being on the radar at the nurses’ station in those wee hours of the morning when a loved one needs pain medication.
However, for those of you putting together food chains for friends, remember that you don’t necessarily need to schedule dinner every single day. Most folks are very generous, and the leftovers begin to pile up. I ended up feeling guilty as I gave away — and sometimes even had to throw away — food that people had so lovingly prepared.
It also frustrated and disturbed me when my kids would lift the foil on the pan and groan, “Not lasagna again!” It’s hard to write this and not sound ungrateful, but if you are going to go to the effort of making someone dinner, try to find out from the point person what others have brought over that week.
Stuffed animals, large objects, and flowers in the hospital are cheery, but they often translate into things that just need to be moved from room to room or take up space in cramped quarters. Consider practical gifts instead, like pajamas, a luxury soap, a new toothbrush, or slippers. A set of thank- you notes is one of the most useful and helpful gifts you can give the patient.
Also, don’t tell the patient or caregiver to call you if they need anything. That puts the burden of asking for help on them. Instead, suggest something specific you can do to help out: a ride for the kids or a sleepover, a dinner brought to the house (without dishes that need to be returned), cutting the lawn, or walking the dog. Make decisions for them on the details as much as possible. This includes whether or not they’d like chicken or fish. Just do it!
8. CHOOSE YOUR WORDS AND ACTIONS WISELY
Resist the urge to repeatedly tell the person, “You are so strong.” They don’t always feel strong, and they don’t want to have to act strong in front of you or hold back tears so as not to disappoint your expectations or impressions of them.
And don’t expect the patient or caregiver to immediately return your phone call or email. All of their energy right now is focused on themselves (if they are the patient) or their loved one and their other immediate family members. They are being interrupted about every fifteen minutes by medical staff of all sorts, they are talking to doctors, undergoing procedures, perhaps worrying about their children or elderly parents, tending to the immediately critical tasks at home, and, overall, being torn in many directions.
With each concerned phone call I got from a friend who told me that they just needed to hear my voice, I felt more inadequate. “Call me,” well-meaning friends would plead into my answering machine. “I have to know what is happening.” All that did was pile one more ounce of guilt and failure on my shoulders and add to my to- do list another thing that I knew I wouldn’t be able to accomplish — definitely not that day, or maybe ever. If you feel the need to reach out in the midst of the crisis, just leave a message that starts with “You don’t need to call me back, I just wanted you to know I am thinking of you.”
Also, don’t approach the family or patient with tears in your eyes or what I call the “sympathy face” (the hangdog look that says “You poor thing, bless your little heart”). This makes the person feel as if they have to use precious energy to buck you up. If you can’t keep your tears or overpowering empathy to yourself, come back when you can or write a note.
After we’d gotten Bob home from the hospital, I made my first foray out of the house to the local YMCA for a swim. I was afraid to face the well-meaning sympathy and curiosity in people’s eyes, and I didn’t want everyone to ask me how Bob was, because I didn’t have a definitive answer beyond “He is healing.”
I was fragile and timid. I hunched my shoulders over so far I was basically hugging myself as I walked into the locker room. All of a sudden, sailing into my personal space with a giant blond mane and more energy than a Dallas Cowboys cheerleader, was a woman who, to this day, I do not know.
“HOW IS YOUR HUUUUUSBAND?” she screamed, eyes bulging with concern. All heads swiveled toward me. I felt ambushed. My heart started beating wildly, and I simply grunted, doe- eyed, and fled out the locker room door. I understood that the woman thought she was being helpful or thoughtful, but I needed to be approached gently and wanted desperately to be treated like a “normal” person, the person I used to be.
9. UNDERSTAND WHERE FAITH BELONGS
In our own journey, faith, family, and friends played a pivotal role in helping all of us to heal. But faith, especially, means different things to different people. And in the midst of a crisis, people often experience a wide range of emotions.
In the absence of just the right thing to say, there are pat phrases others fall back on that can sound downright irritating, especially if a test result or diagnosis hasn’t gone the right way or an individual’s emotional strength is ebbing. Try not to say, “God doesn’t give you more than you can handle,” “Things happen for a reason,” “What doesn’t kill you makes you stronger,” “There but for the grace of God go all of us,” “He or she is in a better place now,” or “There’s a special place in heaven for you.” In fact, scrub these phrases entirely from your vocabulary. The person or caregiver doesn’t want to feel like Job, wonder why God chose them for this particular rough assignment, or envision a handicapped-parking sign in the hereafter. Be sure not to say things that make a person feel isolated from the greater community, or different from everyone else. Also, keep in mind that while spiritual comfort can be helpful to some, it may come off as irritating or overly personal for others. Make sure you know where people stand on the issue of faith before raising it.
When my friend Gretchen asked me to write some tips for her webpage, to help people cope with approaching her after her son’s cancer diagnosis, I gave her this list. She read it, then asked me to take out number 9. She thought it was a bit insensitive to circumscribe people’s good wishes and best intentions. “Just wait,” I said.
Two weeks into her hospital odyssey, she called and timidly asked me to put this tip back in the blog. We had a good chuckle and she vented for a while. Clearly, she was fed up with trying to catalog the reasons why God would ever give a small child a life-threatening disease.
10. BE THERE FOR THE LONG HAUL
In the first days and weeks of a crisis, people come out of the woodwork, flooding you with offers to help, with food and flowers and kind encouragement. This is wonderful, but it can also be overwhelming. The real work begins when all the neighbors have gone back to their own lives, and the patient and family still need occasional support.
Flowers, for instance, are very cheerful in a hospital room. But their effect can be even greater if you wait a few weeks, or even a month or two, and send them to the home. At that time the patient and the family can focus more fully on the beauty of the gift. It is also often a time when they feel as if many people have retreated; there is no one gathered in the kitchen anymore or answering the phone. This simple gesture will make a big difference after the crush of the crisis and will let them know you are still thinking of them. (Those of you reading this who for years have sent flowers to homes and hospital rooms in the immediate wake of an accident or injury, take heart — there are no truly wrong acts of kindness.)
In the midst of our family’s crisis, a wise friend told me to subscribe to the “chit system.” Immediately after a diagnosis or incident, everyone will rush in to ask what he or she can do. “Tell them they have one chit,” my friend Tom said. “And that you will use it. It may be the next day or even two months from now, but at some point in time you will call in that chit.”
It could be as simple as bringing over a pizza or driving a kid somewhere — or as complicated as dropping everything and being by someone’s side, no matter what. Once, I asked a friend’s husband to come over and check our water heater. That used up his chit.
What was great about this concept was that when all the cars had left the driveway and most people had gotten back to their regular lives, I didn’t end up feeling abandoned or clingy. And, hopefully, no one person felt overburdened in the long run.
Plus, it made friends feel that they were needed and gave them a task, even if it was two months from the time they’d offered.
And it made me feel like I wasn’t a beggar, constantly asking the community for various favors. But all of the people who wanted to help eventually had their chance. To be needed in that way is perhaps the greatest honor of being a true friend.
Three years after Bob’s injury, we have all come out the other side, each member of my family. We are all unexpected experts at surviving. We’re no different than so many American families: we’ve acquired scars, opened our eyes, we’ve grown and stretched, we’ve ached and rejoiced. We’ve felt loss keenly, and we’ve counted our many blessings. None of us will ever underestimate the power of love, family, and the resilience of the human spirit. Through it all, we’ve been grateful to have kept our sense of humor and our general optimism intact. We may be messy at the edges some days, but we are a family firmly united at our core. In the end, we are proud to be wonderfully, perfectly imperfect.
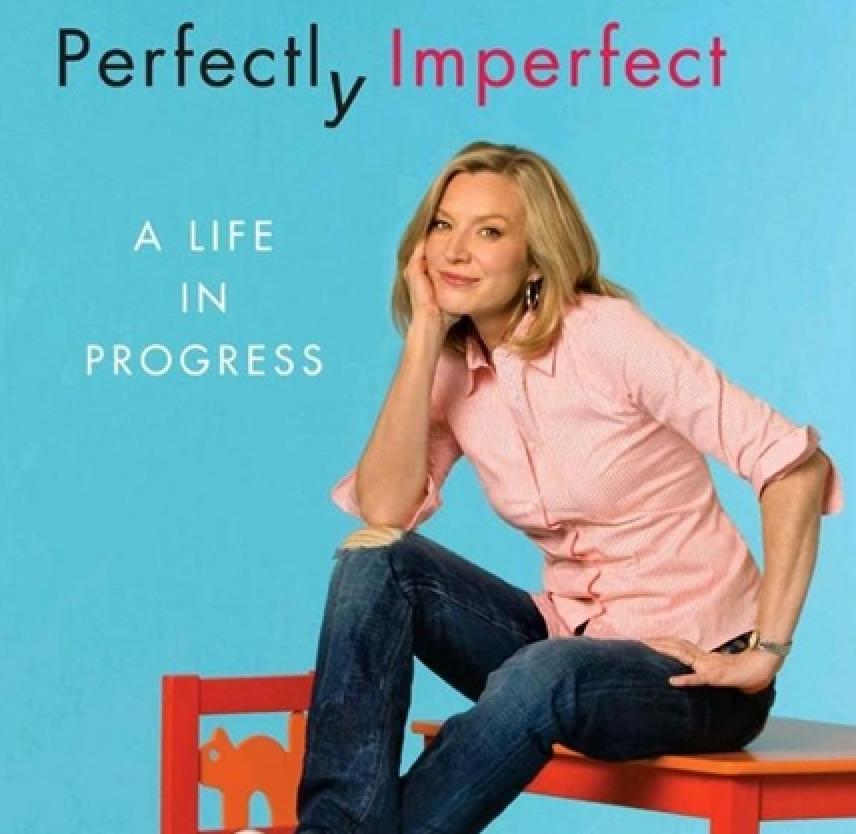
Excerpted from Perfectly Imperfect by Lee Woodruff Copyright © 2009 by Lee Woodruff. Excerpted by permission of Random House Group, a division of Random House, Inc. All rights reserved. No part of this excerpt may be reproduced or reprinted without permission in writing from the publisher.
