Approximately five minutes after a terrible car accident that ejected Matt Trenton from his car, first responders found him face down and not breathing. They placed an endotracheal (breathing) tube in his trachea (windpipe) and transported him to the hospital, where he was admitted to the ICU. He received treatments, such as medications to elevate blood pressure, ventilator support of breathing, and IV fluids for hydration, all of which are necessary to support the brain and the body so that the brain can recover from injury.
Learn more about coma on BrainLine's Disorders of Consciousness Hub.
Although Matt’s vital organs were not seriously injured, a CT scan showed widespread swelling of the brain. Dr. Roberts, a neurologist, evaluated him. Matt was still in the bed and didn’t move spontaneously. When blood was drawn from his arm, he did not move it or even wince. When Dr. Roberts shouted Matt’s name and applied painful stimuli to assess his level of consciousness, his eyes did not open. When she held his eyes open, no spontaneous eye movements were evident, nor did he look at her face. A review of Matt’s medications and the lab and toxicology tests showed the presence of no substances that might worsen Matt’s neurologic exam. Therefore, it was clear that Matt had sustained severe brain damage that was causing severely impaired consciousness—i.e., coma. Matt’s parents asked Dr. Roberts if Matt was conscious or unconscious and whether he was likely to recover. (Note: Matt is not a real patient, but a realistic composite of many patients for whom we have cared.)
In the following article, we present two possible scenarios, discuss how doctors answer these questions, and define the terms: wakefulness, awareness, consciousness, coma, vegetative state, minimally conscious state, and brain death.
A Working Definition of Consciousness: Simultaneous Wakefulness and Awareness
In assessing Matt’s consciousness, Dr. Roberts was not concerned with the notoriously thorny philosophical problems of defining consciousness. She was concerned with assessing the function of the parts of the brain that are responsible for consciousness so that she could determine if Matt was aware of anything and if he was capable of suffering.
Neurologists divide consciousness into two components: wakefulness and awareness. Both must be present for consciousness to be present. The neurons and their circuits (connections) that support wakefulness are in one region of the brain, and the neurons and circuits that provide awareness are in other regions of the brain. Dr. Roberts first had to determine whether Matt’s brain was capable of wakefulness, and then she would look for signs of awareness.
Wakefulness
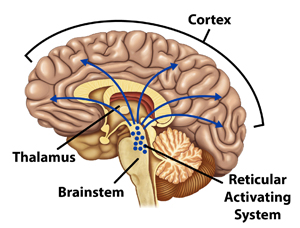
The part of the brain responsible for wakefulness is the reticular activating system (RAS), a collection of neurons in the upper brainstem that sends widespread stimulatory projections to the areas of the brain responsible for awareness. (See figure1.) When the RAS stimulates the brain, a person’s eyes open. Therefore, spontaneous eye opening or eye opening in response to stimuli is a reliable sign that the RAS is functioning and that wakefulness is present. However, although wakefulness is necessary for consciousness, wakefulness alone is insufficient for consciousness. In other words, eye opening alone is not sufficient to indicate that a person is conscious. Clinically, if the RAS is not functioning normally, then the patient is incapable of becoming conscious and the eyes will not open—even in response to painful stimuli (such as pinching the clavicle or pressing a knuckle into the sternum). As a result, the brain is not “turned on” and cannot support awareness. This is much like a computer—if the power supply does not provide electricity to the computer, the computer will not function.
Figure 1.
To determine if Matt was capable of wakefulness, Dr. Roberts examined him for either spontaneous eye opening or eye opening in response to painful stimuli.
Awareness
The parts of the brain responsible for awareness—the ability to think and perceive—are the neurons (brain cells) in the cortex (grey matter) of the two hemispheres and the axons (communicating projections) in the white matter between those neurons. The brain’s neurons are located in the cerebral cortex—the grey matter at the surface of the brain—and in the deep grey matter in nuclei such as the thalamus. These billions of neurons make trillions of connections via axons in the white matter, constituting functional neural networks that support all conscious effort of the brain, as well as many functions of the brain that do not require consciousness.
Awareness is not a function of solely a single area of the cortex or deep grey matter. Rather, it emerges from the coordinated activity of many parts of the brain. Although consciousness is possible with loss of limited areas of the cortex (as can be seen in some stroke victims), severe and widespread injury to the cortex, thalami, white matter, or any combination of these will result in unconsciousness, even if the RAS is functioning normally.
Awareness is tested by attempting to elicit a response to a command that requires some thinking ability, such as “look at me,” “hold up two fingers,” or “try to mouth words.” Awareness can also be indicated by purposeful movements such as pushing away at a painful stimulus; this purposeful response contrasts to the automatic reflex movements that occur in response to painful stimuli when one is in a coma.
States of Disordered Consciousness
In the first scenario below, we consider Matt’s condition in the days, weeks, and months after his accident and describe his states of consciousness, along with what was known about his prognosis. Patients with severe brain injury and coma who recover may, depending on the severity of the brain injury, progress through several levels of consciousness, from coma, to vegetative state, to minimally conscious state, to consciousness, with varying degrees of motor, cognitive, and affective impairment. The range of potential outcomes is wide.
Coma—Neither Awake nor Aware
Two days after the accident, Matt did not open his eyes, make any purposeful spontaneous movements, or respond to Dr. Robert’s commands or to any other stimuli, including painful stimuli. Dr. Roberts concluded that the RAS was not working, and she described Matt as being in a coma—he was neither awake nor aware. She had good reason to believe that Matt was not simply in the locked-in state, which is the state of being conscious but unable to move. This happens rarely after certain types of stroke (which would have been seen on his brain scan), or in the late stages of some neuromuscular diseases.
The presence of coma early after an injury does not predict a patient’s outcome. Patients with widespread injury to the brain are more likely to have severe neurologic deficits and are at a higher risk of prolonged unconsciousness. Patients with more focal injuries (for example, only a brainstem injury) may have less severe neurologic impairment and are more likely to have a temporary coma. The nature of the neurologic impairments depends on the areas of the brain that have been injured, and Matt’s injuries were uncertain. Although his brain CT scan did not reveal major structural injuries, he may have suffered (1) widespread injury to the neurons of the cortex and thalamus because he was deprived of oxygen and (2) injury to the white matter because of the physical forces of the traumatic brain injury.
Although the RAS was not functioning normally, Dr. Roberts found that other important brainstem areas were still functioning. Matt’s pupils responded to light, his eyes blinked when his eyelashes were touched, he gagged when a suction catheter was passed through the endotracheal tube to his lungs, and he was initiating breaths on his own, even though he required support from the ventilator. The presence of these brainstem functions was favorable but did not indicate whether he would eventually recover consciousness. Although he had spontaneous breathing, he could not swallow safely or protect his airway from aspiration (sucking liquids into the lung), which would cause pneumonia; therefore, he needed the endotracheal tube. He also required a nasogastric tube into the stomach to receive a feeding solution for adequate nutrition.
Coma usually lasts for no more than two to three weeks. In most instances, coma evolves to the next level of consciousness, known as the vegetative state.
Vegetative State—Awake but Unaware
Unless the RAS is severely injured, its function returns in two to three weeks. Ten days after Matt’s accident, his eyes began to open in response to painful stimuli, which implied the presence of wakefulness and that spontaneous eye opening would eventually occur. However, despite the fact that his eyes were open, when Dr. Roberts called his name or placed her face close to his, Matt did not look at her, which indicated that even though he was awake, he was not aware of her or of his surroundings—i.e., he was still unconscious. Similarly, his motor responses to pain consisted only of reflexes and not purposeful movements. Note that although patients in a vegetative state have reflex responses to pain, because they are not conscious, they cannot experience either pain or suffering. Therefore, Matt’s condition was defined as the vegetative state, a condition that may either be a temporary stage in recovery from a coma or may be more longstanding if the brain injuries are severe and irreversible.
Endotracheal and nasogastric tubes that are placed when patients emergently enter the hospital can remain in the body for only a limited period of time because they may cause injury to the larynx or stomach over an extended period of time. However, patients in a vegetative state, like Matt, are incapable of protecting their airways or of taking oral nutrition and hydration. Therefore, a more permanent breathing tube, called a tracheostomy, is surgically inserted through the front of the neck directly into the trachea, and a semi-permanent tube, known as a gastrostomy tube, is inserted directly through the abdominal wall into the stomach so that the patient can receive nutrition and hydration.
Two weeks after his brain injury, Matt’s prognosis was still uncertain. Dr. Roberts told Matt’s parents that in the best case, he would regain consciousness but would likely have severe, permanent physical and cognitive limitations. In the worst case, he would never regain consciousness. Matt’s parents, not wanting to give up prematurely and hoping that he would eventually “wake up,” elected to have the tracheostomy and gastrostomy tubes placed.
Persistent Vegetative State
Six weeks after Matt’s accident, he was breathing through the tracheostomy without the support of a ventilator; however, he still required the gastrostomy tube for nutrition and hydration. He was transferred to a rehabilitation hospital, where Dr. Roberts examined him again and found that he was still vegetative—awake but unaware. By convention, after one month, the vegetative state is described as the persistent vegetative state (PVS). Dr. Roberts explained to Matt’s parents that the term “PVS” does not stand for “permanent vegetative state” and that Matt’s long-term prognosis was still uncertain. Because patients may emerge from PVS, usually within 3–12 months, clarifying the distinction between persistent vegetative state and permanent vegetative state was important.
Matt’s parents asked Dr. Roberts about Matt’s odds of recovering consciousness. The most important factor influencing the likelihood of recovery is the type of brain injury a patient has suffered. Patients in the PVS after a traumatic brain injury can regain awareness as late as 12 months after the injury; however, after that, the likelihood of recovery is very slim. The prognosis with a brain injury caused by hypoxic-ischemic injury (lack of blood flow and oxygen) is worse than that with an injury caused by trauma. Common causes of hypoxic-ischemic injury are cardiac arrest and drowning. Patients with hypoxic-ischemic brain damage are very unlikely to recover any awareness after only three months in the vegetative state; and among those who do, a good neurologic recovery is very rare. Age is also an important factor. Younger patients have a higher probability of recovering consciousness early on; but after 3–12 months (depending on the type of injury), even children are extremely likely to remain in a vegetative state.
Matt’s brain injury was a combination of traumatic and hypoxic-ischemic injury because he was not breathing immediately after the accident. As a result, at six weeks after injury, the odds of Matt recovering some consciousness were small but not impossible. However, if Matt remained in the PVS at three months, his odds of recovering consciousness would be extremely poor, and Dr. Roberts would be able to say with a high degree of certainty that Matt would not have a good cognitive or functional recovery.
The Minimally Conscious State
Nine weeks after the accident, Matt started responding—just a tiny bit—to examiners and his environment. His caregivers noticed that if his eyes were open and someone called to him, his eyes would often, but not consistently, look in the direction of the voice. Sometimes, if his blood was being drawn, he would moan or grimace or weakly pull away from the pain, in a purposeful nonreflexive way. His parents had also seen him attempt to mouth words, but he did not do so on a consistent basis.
Matt was showing possible signs of consciousness, but his degree of neurologic functioning was not sufficient for him to communicate his needs or to care for himself. His condition had progressed to the minimally conscious state (MCS), which is characterized by either minimal or fleeting and inconsistent responses that nonetheless are consciously driven and represent more than the reflex responses seen in a coma and the PVS. Some patients in the MCS progress to have consistent awareness, whereas others continue to fluctuate between the PVS and the MCS. In some sense, the MCS is better than PVS because it suggests that some parts of the cortex, thalami, and white matter are working in a coordinated fashion. However, in the MCS, Matt was able to perceive his pain and his circumstances but was unable to communicate to others about his experience or his own perception of his condition. Because his MCS was the result of such a severe and widespread brain injury, Matt still needed the feeding tube for nutrition and hydration, and meticulous nursing care for all of his physical needs.
After Matt emerged into the MCS, his parents were hopeful that he would continue to improve. Sadly, after three more months, he had not. He continued to fluctuate between the PVS and the MCS. Dr. Roberts informed Matt’s parents that the likelihood of a good recovery—meaning that Matt could communicate his needs and make useful movements with his hands and arms—was exceedingly low. Although she could not rule out the possibility of minimal improvement over months or years, she could say that he would never be able to care for himself or engage in complex social interactions.
Matt’s parents considered whether Matt would want them to continue tube feedings in his current condition without a reasonable chance of a recovery that he would think was meaningful. After many discussions with their family, friends, social workers, and clinicians, Matt’s parents concluded that he would not have wanted to continue treatment, and they asked that the tube feedings be stopped. This request was honored, and nine days later, Matt passed away without evidence of pain or discomfort.
Brain Death
In the previous scenario, Matt progressed from coma to the vegetative state to the MCS. However, rather than improve, some patients in coma worsen. In the following alternate scenario, Matt’s brain injuries were much worse than described above, and the clinical course differed significantly.
Two days after his accident, Matt was comatose and had no brainstem reflexes. His pupils did not respond to light, his eyelids did not blink when his eye was touched with sterile cotton, he did not have a gag or cough reflex in response to tracheal suction, and he did not initiate any breaths on his own—all breathing was provided by the ventilator. Dr. Roberts concluded that Matt had suffered a severe and potentially irreversible injury to all of the neurons in his brainstem, cortex, and thalami and that his condition was probably worsening toward brain death, a term that refers to the irreversible loss of all clinical brain functions, including all brainstem reflexes and the drive to breathe.
To confirm brain death, Dr. Roberts performed a series of formal tests known as the brain death examination, which is recommended by the American Academy of Neurology to look for any brain function. This examination confirmed that Matt was comatose and that he lacked all brainstem reflexes, including the respiratory drive. When the ventilator was temporarily disconnected from the endotracheal tube while his vital signs were being carefully monitored, Matt made no effort to breathe--even when the carbon dioxide level in the bloodstream reached levels that normally elicit gasping and breathing. Following her hospital’s protocol, six hours later, Dr. Roberts performed a second brain death examination, which elicited the same findings.
As is the practice in the U.S. and many other nations, Dr. Roberts pronounced Matt dead on the basis of brain-death criteria. She explained how she made this determination to Matt’s parents and told them that the ventilator and any fluids or medications would soon be stopped, once they had had a chance to say goodbye.
In accordance with hospital protocol and national standards of practice, Matt’s parents were told about the possibility of organ donation. Patients pronounced dead by brain-death criteria have the opportunity to donate all of their major organs (kidneys, liver, pancreas, intestines, heart, and lungs) and tissues (cornea, skin, bone) because the organs and tissues can remain viable for transplantation until the ventilator is stopped. Matt’s parents believed Matt would want to donate his organs, and after discussion with the regional Organ Procurement Organization, they agreed to the donation.
Cochrane, T.I., & Williams, M.A. (2015) Disorders of Consciousness: Brain Death, Coma, and the Vegetative and Minimally Conscious States. New York: Dana.
From the Dana Foundation. Used with permission. www.dana.org.

Comments (88)
Please remember, we are not able to give medical or legal advice. If you have medical concerns, please consult your doctor. All posted comments are the views and opinions of the poster only.
Barbara replied on Permalink
At age 2, I fell 2 stories onto concrete and was comatose for 4 days. It was 1954. I have lived all these years not understanding why I have moments of rage, occasional panic attacks, depression and anxiety. I've been treated for these on and off for years but no clinician ever asked me whether I experienced any brain injury. A new friend has a son who exhibits my issues as a result of a traumatic brain injury. Hearing about his personal and emotional issues, inability to hold job, difficulty in relationships, impulsiveness too, I realize that while I thought my problems were genetic, they really come from that horrible fall at age 2. Now, I'm able to tell my children this isn't genetics. I'm relieved but sad that all those professionals I consulted over the years never thought to ask me about my childhood. I look normal; most of the time I act normal but I know my thoughts processes are challenged. And it's not anything I can change because some parts of my brain were damaged, may have died. So my emotional development is compromised. Thanks for this article. I'm trying to find other adults who had similar childhood trauma.
Joyce replied on Permalink
My friend has a THI appx 30 years ago’. Car related accident. He was in a coma x 3days. In 2018 he had most of his teeth surgically removed due to gum disease. Next morning at home he had a cerebellum stroke. Took one year to be able to walk well. He is now 65 yrs old. He has had 5-6 falls that i know of in the past 4months. Back of the head laceration, and 2 facial laceration, bridge of nose and eyebrow lacerations. He has anxiety and panic attacks that he is aware of and is apparent. He loses his temper easily and rants. He has trouble being organized. He loses his phone , glasses, wallet and other items daily. He was a brilliant criminal defense lawyer prior to the first accident. He actually won a Supreme Court case and has a Wikipedia page. After the stroke he has delivered pizza and washed dishes in restaurants. He has not followed up medically since 2018 stroke. I met him a year ago. He had no medical insurance. I have assisted him in getting Medicare and Medicaid coverage. He is resistant to seeing a doctor for evaluation. Could he be having brain damage still occuring? Trying to get an appointment with a specialist is weeks to months out. I am very worried about him. Comments and suggestions please!
Kunior replied on Permalink
I've been searching for sumthing anything that can give me sum kind of answers November 29th 2021 I was in a serve car wreck ejected from the vehicle big lash on forehead broken collarbone broke T8 T9 T10 in my spine broke 3 ribs also punchared lung not to mention my neck issues. So from November 29th till December 19th I was out of conconsciousness even when I woke up it was crazy I guess I could hear the nurses sum what because they would talk to me while I was out because when I woke I already knew everything that was wrong with me and what happened to me it was weird... Also I'm the 20 sumthing days I was in a coma I had the most vivid dream sumtimes i.could see things other times it was just pictures black with a scary sounding voice like telling me awful things all I remember was I just wanted to wake up so bad so I didn't have to hear that voice.. it's hard to explain I was so desperate for water it was unreal I was so thirsty I couldn't believe it . I really just wanna know if anyone ever experienced anything close to this there's so much more I went through but if anyone wants to talk more about what happened or what you went through maybe we can share our stories
Tiffany Mckee replied on Permalink
Hi nilly 13 years ago my life changed i had poast natel my husband and son I left for a monster who hurt me I can't remember what happened iv been told and the police say im lucky I can't remember let's just say he use to bash me until I was unconscious my family new something bad was going to happen to me iv always been a tomboy but being hit by a man double ur size and he was on drugs i had no chance
Then one Wednesday afternoon my mum who was preparing a rost for dinner got a call from the goldcoast hospital looking for a tiffany my mother said no that's my daughter then they said we think tiffany has had a accident could my mum come to the hospital to identify this women who was fighting for her life
They didn't let my mother in yet until they new it was me
Some how I landed off a balcony in surfers paradise I fell on my head 18 metres onto concrete let's say I broke lots of bones lost a lot of blood and needed help breathing
I was rushed to hospital and put in an induced coma for 2 months
When I woke I had family there I didn't know what had happened I thought I'd been sky diving from my accident I have an inquired head injury and front lobal damage and I suffer from PTS and no one has been charged its an on going thing
Domestic violence wasn't talked about 13 years ago I feel iv been ripped off no one will ever know the truth
I wish I had my life back
Bonnie hamby replied on Permalink
I read your post and just wanted to say I am so sorry for what you've been through and I hope everything gets better for you as I will pray for you.
I my self was kidnapped raped severy abused poisoned drug behind a truck left in the trunk of a car tied up in the woods for day and shot 3 times in the head by my ex child hood best friend.. the person who I thought I could trust the most was the one person I couldn't trust at all and who severely hurt me and left me for dead..
Marcusly I am alive thanks to the Lord the Lord saved my life that day when I needed him most, at the right second and just at the right moment he saved me I didn't ever thank the Lord loved or cared about me but he actually does and I am living proof that he is real and can hear us, save us protect us guide us as he loves forgive everyone of us no matter what we've done wrong. We just have to ask him for help except his help pray and
talk and walk and believe in the Lord everyday. I strongly believe if the Lord can help and save me then he will help and save anyone who ask excepts and believes in him.. I also believe the Lord saved you to.. I know we don't have exactly the same story but we've both been hurt, therefore I believe we both will over come those terrible times and rise to the top because the Lord has special plans for us both.. things will get better for you I guarantee just pray every day and talk to the Lord as he will guide u n protect u n save u like he's been doing. I'm here if you ever need anything my name is Bonnie Hamby my email is 06071964b -at- gmail incase u need to reach me or u just need a friend to talk to . I'm here for u . I wish u the best as u recover and get stronger everyday that goes by.. I will end my message but never my love.. hope to talk to u soon new. Friend.. your a great person I can feel it so never forget that ok and God loves you as well as I do n were always here for u nomatter what.. sincerely Bonnie hamby
Anonymous replied on Permalink
I was in a coma for 8 days and my passenger said my eyes were open and couldn't tell if I was awake or not, so if someone isn't responding but they're eyes are open they probably aren't conscious and need medical attention asap
Anonymous replied on Permalink
Is it possible for a person to still hear you or have their hearing if they have minimal brain fuction?
Anonymous replied on Permalink
reading this was really creepy; I've been involved in a car accident which caused me a severe brain contusion and a coma which lasted twenty days and the way I reacted to any kind of medical care was exactly the same as described above. I was desperately looking for a similar situation to mine on internet, for i have - for a long time - really wanted to confront with someone who lived through the same experience that I lived. I have often managed to talk with people who have had an head trauma, but their situations had been a lot less serious: a shorter time of unconsciousness, lighter neurological consequences, and so on. I'm glad I found a description of my own experience, but I still long for a person who has lived what I lived.
Heather replied on Permalink
My brother is going through this, waiting for him to awaken.
Relle replied on Permalink
Hi - 31 years ago at age 18, I was hit by a motorbike and was in a coma for the next 3 months. I also had the gastrostomy tube for feeding and a tracheostomy for breathing. I started to slowly wake but had a concentration and memory span of only seconds and was transferred to the rehab wards soon after. I needed extensive physio for regaining balance and the ability to walk again, speech (I spoke too fast and slurred) and occupational therapy (for seized left elbow and fine motor skills) for 6 months before my discharge. The following year, I returned to university to complete my science degree in biochemistry that I had started the year I had my accident and completed it in 4 years. I found over the years that I have always had a memory problem but I found ways to work around this. One thing I didn’t like was other people’s judgement. I have always been fiercely independent so would find it difficult to ask for help. I have recently been diagnosed with autoimmune hepatitis and I was trying to find any link with past TBI’s and liver disorders and came across this site. I have also been diagnosed at age 40 with osteogenesis type 4 affecting my tendons, cartilage and collagen and thought that the pain in my hip joints were a result of the accident. I too have longed to talk to someone who is similar to me who has overcome the hurdles thrown in the way. I wrote a book about my accident and life straight after about 8 years after the accident and found this to be extremely therapeutic. It helped me deal with my obsessions and anxieties created by the accident - I haven’t published it yet but have given it to friends and family to read (and return). I can’t stress how important this step was to my acceptance stage of my recovery.
Vee replied on Permalink
I am so glad u recovered. My nephew is in a coma from a MVA brain injury. Today is day 7. You give me hope. Thank you and God bless.
Shawn replied on Permalink
Please hang in there and don’t give up hope. I’ve been through all of this and had my traumatic brain injury when I was severely beaten by three men stomping on my head. Thank God I don’t remember feeling any pain but I went through all of the above stages and don’t remember anything until I saw my mothers face three weeks after the incident. Telling her, “Mom I wanna go home” just moving my lips as my jaw was wired shut. I’m 40 now and this happens in 2004 (24 years) but it still makes me cry talking about it. I’ve made a full recovery and I’m sure that I scared a lot of my friends and family but just keep praying and the human body is very powerful and it takes a lot to end it
Sonica replied on Permalink
hi, my cousin had a very bad car accident last week Thursday. The last 5 days she’s been unconscious and the doctors have said her brain is all damaged... her lungs are also not great. She’s on a ventilator.. any advice.. I’m not sure she will make it she’s very young 29. I have no idea what to do as there is nothing we can do for her but wait. This is the 5th day of waiting!!
COLEEN DEROBERTS replied on Permalink
Hi there Anonomys,
I totally understand you need to connect with some one who has gone through, and survived, as traumatic brain injury as serious as yours.
My 30 year old son left my house with 6 angry parametics, who freely informed me that the were, "Sick of this shit", because they had be called 2 and 4 weeks prior for what we assumed were overdose related respitory failure.
This occurred on March 30th, 2020, the day the hospital closed it's doors to visitors.
Even though I followed the ambulance to the ER, I was not allowed to be with my son due to Covid-19 no visitation restrictions.
This provided the perfect storm. I could sense that this had some how become a life-or-death situation. Everyone was screaming inside the ER. The EMTs never left, they just walked in and out. One of them seemed pretty upset. The hospital's security guard was so pumped up with adreneline that the man ran up to me as I was quietly praying on the bench he ordered me to sit on and not move from, and put his finger in my face then yelled, " Look lady, I'm sick of your shit!"
I was speachless. I said, "What???... I thought you were supposed to give me a yes or no anwer from the request I had made to Administration through the Patient Advocate if I could go in the ER to be with my son."
Then he said the same phrase as the last parametic who slammed my front door closed after stating, " Wer're sick and tired of this bullshit!"
Alarms and red lights went off in my head, just before this weird man grappled me into some kind of upsidewown hold, and continuously changed his grasp in order to inflict as much pain as he could as he carried me about 15 feet. Finally, I was able to struggle free and scream, "How dare you! How dare you put you hand on a 51 year old woman like that and intentionally hurt me!"
Then I thought, "Oh God, this guy is unstable and he has direct access to my son. He may have attacked me because he's already hurt Jesse.
So I shut up and quickly left without another word.
Hours later I called to find that my son, who left our home in perfect health, but defenseless in a state of hyperventilation, was in the Neuro ICU with anoxic whole brain injury, and lying in a coma.
WTF happened to my kid? Its day 45, he wakes up and can make meaningful eye contact with me and the family, even with the loving caregiver who speaks spanish to him. But then sometimes he just stares. Then he's back. But can only move his toes and hold up his neck. Do you think from your experience that he can improve?
Thanks honey. I'm so sorry for your pain. I know even minor head injuries will leave you with memory deficits (that's me). I know he's angry about what happened to him and remembers, I know he relaxes only when I sooth him. But the muscle seizures or spasms are frequent and continuous if I'm not there. Do you remembera feeling pain???
Anonymous replied on Permalink
Hi, I read this article and my boyfriend was in a critical car crash, and his situation is very similar to how Matt's was described. He is completely recovered now and has all his cognitive functions but minimal hearing problems in one ear and nerve damage on half his face. I am extremely sorry you went through I totally understand. Praying for everyone
Emily replied on Permalink
I have been looking on the internet for the injury I had too and I can't find much about it. There's a lot on mild TBI and CTE but not a whole lot of the outlook of severe TBI and coma. My situation wasn't as severe as yours, I was in a coma for 9 days, when I woke up I had post traumatic amnesia, I couldn't understand that I had been injured and claimed I was fine, and I kept saying I was in Florida or Arizona (I live in Michigan). I was behaving like a toddler as well. I don't remember a whole lot, this is what I know from my medical records and the information my mom gave me. It's been 5 and a half years and I feel like my mental state is declining. I keep screwing up due dates for homework, overlooking important information, my visual disturbances got bad in 2018 it's flickering little bright spots in my vision field, my depression worsened at the time, got better s little bit (because I was drinking every day so I don't know how much better) and then 9 months later it got bad again and it's been a year, so I'm trying to find out what this all means because I've seen 5 doctors and the best diagnosis I got was depression and lateral heterophobia. Anyway, I'm glad you're doing better now.
Shawn replied on Permalink
I can totally remember the toddler state of having a brain injury. I don’t know if it’s because I was heavily medicated with tons of morphine for my pain or the cognitive state that my brain was in but the child like characteristics are definitely noticeable in a brain injury victim
Roz replied on Permalink
I just read your comment, my situation is most likely similar t9 yours. Lmk if you want to talk.
Cheryl replied on Permalink
My sister survived a tragic car accident when she was 17 years old. She was in a coma for months. Eventually came out of the coma, couldn't talk and learned to communicate by use of an alphabet board we made for her. She would spell out what she wanted to say. Had to learn how to walk again with lots of rehab she can speak and walk with the use of a 4 pronged cane. 50 years later and she now uses a motorized wheelchair.
David Burch replied on Permalink
Was in major car accident, at time unknowingly suffered tbi , wrongfully accused and arrested of DWI, due to altering effects of consciousness..
Ponzi replied on Permalink
Hi, I have a friend who was in a terrible motorcycle accident in January and has been unconscious since then, it is now mid/late April. He has had a couple small instances that he seemed to vocally respond however he has not done so in about 2 weeks. He is no longer on a ventilator and is breathing on his own but that is all he is able to do. They are able to wheel him outside and was in hopes that the fresh air and sun would help since he was a very outdoorsy person before the accident. They did have to remove a small section of his brain due to blood loss but I am unsure of what part. Since he has been unconscious for nearly 3 months, what would the likelihood of him waking up at all be?
Beth replied on Permalink
Definitely possible. I heard of someone who was in a coma for 19 years and they regained consciousness. Whilst three months is a considerable amount of time for a coma, there are people who have been in a coma for way longer and still survived.
It's late Decemb
Yogini Joshi replied on Permalink
Very well explained. I have a relative in ICU currently and this information helps
Georgette replied on Permalink
Thank you for this article. I was looking for research on brain injuries due to car accidents for my new novel. I appreciate that you used a real life scenario. It helped me to understand and follow along. I'm excited because know I can make my story realistic and believable based on how you wrote this in laymen terms. Thanks again.
Pete Simpkin replied on Permalink
I feel for anyone with a head injury, I really do. The uncertainty of a head injury
and its outcome Is the main concern here I think.
The darkest day of my life occurred one normal sunny day when I was riding my
Motorbike and I collided with a car which turned into my path. What happened
Next is extraordinary as I was probably thrown up into the air and when I hit the
Ground my helmet was completely knocked off my head with such force I was
Knocked Out. This was incredibly dangerous. I will never know if the helmet
Failed me or it was just a freak accident.
As I lay Unconscious on the road people from nearby houses and passing cars
Would have stopped and helped, prior to the arrival of the police and paramedics.
I don’t remember anything about the police, paramedics or helpers attending to
me. For around 40 minutes I remained unconscious with absolute minimal memory
of anything.
There was just 2 very, very brief moments when I vaguely remembered anything
At all. It was mostly just darkness and silence, like being shut away alone in a
Dark, Silent and empty room. I never woke up again till I was in Hospital
When I regained consciousness in hospital it felt like I had been asleep but for no
Reason.
The helmet coming off has troubled me and puzzled me since and I believe I
Was Knocked Out by the sheer force transmitted to my brain from a blow to the
Base of my skull/jaw from the helmet being knocked off my head. I broke a tooth
That supports this theory.
I had a friend on the back of my bike who said my helmet just laid in the road as
although he was injured, he was conscious and he told me later what had happened.
He told me I was Unconscious and “Out Cold”.
I was shocked and you never forget the day when your life is turned upside-down
In a few seconds. I was just 18.
Even riding safely with a helmet doesn’t guarantee prevention from a serious
Concussion.
Michael replied on Permalink
I’ve had 4 concussions that caused me to loose consciousness. Two of the Four (kicked by horse in head and car crash) I lost consciousness for at least an hour. I’ve had numerous minor blows to the head that made me feel dizzy, nauseous and sleepy. I’ve been diagnosed with ADD should I go see a neurologist?
Lesley replied on Permalink
You know the answer to this question. Since this is an old post I hope you have already done so. The answer is yes.
Valerie Heike replied on Permalink
Back lower left quaddrant feels like that part of my head moves
Sometimes when I smile I have brief swver pain. Firemen in December 2014 in Waukon IA slammed my head into the wall getting me out of the den when my half sister set our laundry room on fire. My head was swollen for nearly two years.
Jennifer replied on Permalink
My TBI happened on 07/03/2001. I was in a coma for 2 months. Still to this date I still suffer from a good sized list of problems. My frontal lobe was destroyed. I've been told by Dr.'s I'll never fully recover. I've got a lotta hate.
jack replied on Permalink
Karen is right ... Hate is like a cancer that consumes YOU from the inside out. I recommend to study the Bible & visualize the TRUTH of it that your spiritual connection to Jesus is the only thing that really matters in this life. Life on this earth is like a six pack of beer compared to the OCEAN (that is the ETERNITY which follows after this brief and USUALLY unpleasant life) ... way too many people are missing that REALITY. I HOPE you do not join them.
Courtney Mansell replied on Permalink
I just wanted to thank you for sharing... I really needed to hear this ... Having had a TBI 4 years ago myself, n am now just trying to stay positive and hopeful for the looove of my life who suffered a cardiac arrest unresponsive not breathing for atleast 10 minutes..but quite possibly longer as he was in jail when it happened.. He has been in the MICU for the past 4 days in a coma ventilator while also being placed in a state of hypothermic protocol which is supposed to help preserve or atleast stop further damage to his brain and all the rest of his vital organs. He is being warmed ATM and once he reaches the correct core temperature hes scheduled to then have MRI and scans done to see if there is any improvement to his current comatose state. EEG showing stable and today when he was being suctioned his body showed signs of hope atleast thats how I percieve it to be .. By coughing while being suctioned. Power of prayer and manifesting and showing unconditional love and feeling like if I dont give up on him HE WONT GIVE UP on me is what has gotten me through this horribly tragic scary and all too traumatic situation up to this point. Please anyone that reads this... Say a prayer for him.. HIS NAME IS MARSHALL BRADBERRY and he completes me and tbh I dont wanna be apart of this world if hes not going to be here with me by side. HE - WELL WE BUT MARSHALL NEEDS ALL THE POWER OF PRAYER THAT HE CAN GET!! I LOVE YOU ALL AND FEEL FOR YOU ALL AND ALL I CAN SAY IS THANK YOU. YOU MATTER. YOU ARE IMPORTANT. AND ALWAYS REMEMBER NO ONE IS PERFECT AND LOVE HEALS ALL. THANK YOU. GOD BLESS.
Karen L replied on Permalink
Please work on losing the hate..It’s hard... but it’s draining your good energy to use in being happy. Life is unfair, it can suck, but you’re alive and there’s a world full of new people and experiences if you open yourself up to them. So, forgive for your sake.
Anonymous replied on Permalink
I am reading this because I suffered a brain injury and had all the symptoms from getting hit by a Tractor Tailor. I was rushed to the hospital only for them to give me medication that didn't help. They didn't perform any test just asked me my name and what happened.... I don't know what to do because I am progressively getting worse (I'm 16 years old by the way)
Cathy replied on Permalink
I truly fell deeply for all here I am a victim of a road rage attack and rear 80mph impact I am alive and greatful but I will never be the same ,and will never have my quality of life back. I have spent 3 years trying to find be up for this horrendous pain in my head and neck without having to take so many pills. :'(
jack replied on Permalink
I recommend to study the Bible & visualize the TRUTH of it that your spiritual connection to Jesus is the only thing that really matters in this life. Life on this earth is like a six pack of beer compared to the OCEAN (that is the ETERNITY which follows after this brief and USUALLY unpleasant life) ... way too many people are missing that REALITY. I HOPE you can overcome the "unhappiness" of the pain this life has handed you and just focus on the JOY of ETERNITY which YOU HAVE THE POWER TO OBTAIN.
Anonymous replied on Permalink
Hi My partner was in a car accident 3 weeks ago and when the weather got warmer over 75F he starts to overheat. If he doesn't get out of the warmth he gets the concussion symptoms back of , headachy, brain fog, and very tired. Asked two doctors now and both say not normal. Anyone have any suggestions?
Anonymous replied on Permalink
Anonymous replied on Permalink
My husband suffered a terrible accident and caused trauma in the brain and he got surgery and they placed his bone back. My mother in laws says that he hit pretty hard and that he will never be the same person. Is that true? Do injuries like this cause the person to stay the way they are or is there a chance that they can be normal again?
Anonymous replied on Permalink
I had a bad accident in '97. I was going 20 mph on a bicyicle when a woman pulled in front of me. My face distroyed her side mirror which did the same to my face. Every bone in my face was splintered in a thousand pieces. Both jaws were knocked loss, my eye was hanging out, my skull was cracked and I had a bad concution. The doctor said I had little chance of survival and if I did I would be blind. Miraculously I survived but it distroyed my ability to love. I whisk I had died.
Anonymous replied on Permalink
I'm sorry to hear about your mom. My brother was attacked and hit in the head several times. It's a nightmare. So I'm praying for you!!! But a nursing home isn't that much different then a hospital and if the hospital says she can't stay a nursing home is the best place to put her. They can give her round the clock care she needs. So I know it's tough to think of but unless you can afford to have round the clock care if you kept her at your home. But if you don't a nursing home is your best option. It' also has less patients then a hospital so she would be in good hands!!! I really hope this helps you out... May the Lord bless and keep you, your mother and family!!! ðŸ™ðŸ¼
Anonymous replied on Permalink
Don't take her to a nursing home. Fight. She will not get the care she needs in a nursing home. The insurance companies just want her out. Keep her in the hospital.
Anonymous replied on Permalink
My husband was in an accident and got a very bad brain injury and put in a coma for 7 days that he wasn't supposed to wake up from, doctors tell us he is a miracle. He suffers from major mood disorders and major bipolar disorder. He is a sweetheart one minute and a mean person the next. We have tried several medications and currently he is on Latuda, it was working at first and now it seems that he's so immune to it that it doesn't work anymore. I have been recently doing research to see if his brain can be surgically fixed, but haven't really found anything that's stuck out. I want my loving husband back, what do I do, what is the next step to try or path to go down?
Hope Erwin replied on Permalink
I never realized how the seriousness or the depths of brain injury. Almost three tweaks ago my boyfriend had an accident and was in a Coma. His prognosis was not good, with Dr reports stating he had brain damage, so even if he'd survive, he would never walk, talk, or take care of himself. Well he was a miracle and the Lord spared his life. I received the good news and was so ecstatic, he's talking, remembers people and is feeding himself and his walking is progressing everyday. It's amazing!!! The only issue I'm having is, it is just not the man I knew before the accident. His brain functioning isn't working properly. While he knows what's going on, and what happened to him, he's familiar with family, friends and is before life, he always thinks he's in different states and locations, it's like he's emotionless, and lifeless. I go visit and it's devasting me daily. He knows who I am and talks to me, but he was an extremely affectionate, caring person, we were unseparable, now he doesn't show any emotions or affections. It's like I'm a stranger to him and when I call he just wants off the phone. Is this normal or could he of just lost his feelings or awareness of them? Sounds similar to what your experiencing with your husband's moods.
TheQueen replied on Permalink
My husband is reacting the same way,he notices us family but mentally he is not ok.He says weird things,gets off topic,doesn't remember much about us(though aware who I am),not aware of where he is,his job and where we live because currently we are away from home in another city where he was admitted last week he's clueless that he is in hospital.I worry about his mental state,a lot.
Ssh359 replied on Permalink
I had a concussion years ago from a rear end accident & I remember feeling absolutely flat like I had no emotions. I actually went out and got a dog for the first time in my life. The love I felt brought me back to feeling emotions again. So my advice would be stay affectionate with your boyfriend, show him how much you care & eventually his brain will heal & his emotions & feeling for you will come to the surface. Be patient & loving.
Siboniso Zungu replied on Permalink
Hi, After How long ?
I have a friend who was involved in an accident on the 1st of December 2018, He is still in ICU has never woken up since the accident and the doctors don't know what's wrong
with him anymore.
Hope Sherman Gu... replied on Permalink
I've had three brain injuries in the last 40 years. The first in a car accident left me unconscious for 24 hours. There was no treatment in the hospital, not even cleaning my head wounds and removing the broken glass. The next two were in 78 and 2000. They were much less serious, but the third left me with diminished short-term memory, inability to focus, diminished spatial sense, impulsivity, sudden mood changes, and having to talk my way through things like stopping at a stop sign. I did some neurofeedback which helped a lot. I wasn't able to continue, and my memory problems persist, although being now in my 70's doesn't help. I would definitely recommend neurofeedback. I had studied it, myself, prior to third injury. After that third concussion my brain wave patterns had changed dramatically. A certain degree of improvement is definitely achievable with neurofeedback. Good luck.
Anonymous replied on Permalink
In response to January 24th question. There are a list of tests that can and should be done to assist in the diagnosis and decisions for people diagnosed as vegetative. The issue is hospitals are put on tight time lines anymore. I read a study that shows that over 40% of TBI patients in nursing care are misdiagnosed as vegetative when they are minimally conscious. Decisions are forced to be made too soon and with not enough information to do so in many cases. Go to journeyforjessica.com and I would be happy to send you any information and/or contacts I have that can help you.
Anonymous replied on Permalink
I had a car accident two weeks ago. I had pain in my head and felt unwell. I thought it might be because of injury. I had my CT scan done and they found blood in the right side of the brain. I feel very sleepy and get pain in my head. The doctors are going to perform surgery tomorrow to take the blood out. I hope I get normal again
Anonymous replied on Permalink
Your comment stood out to me about your mother, please don't lose hope! My mother on January 25, 2016 suffered from extensive brain damage and was in a coma for two weeks then she was in a locked in state couldn't move an inch of her body and was well unaware. She had a trach and feeding tube and was sent straight out to a nursing home becasue we had no choice due to insurance purposes. It's Febuary 2nd and my mom is going home Wednesday February 8th it has been a long slow process, but God has healed her tremendously she is not 100% back but she no longer has a trach she feeds herself and can walk with a walker. There is always hope!
Pages