What happens to the brain at the point of injury?
Traumatic brain injury (TBI) refers to damage or destruction of brain tissue due to a blow to the head, resulting from an assault, a car crash, a gunshot wound, a fall, or the like.
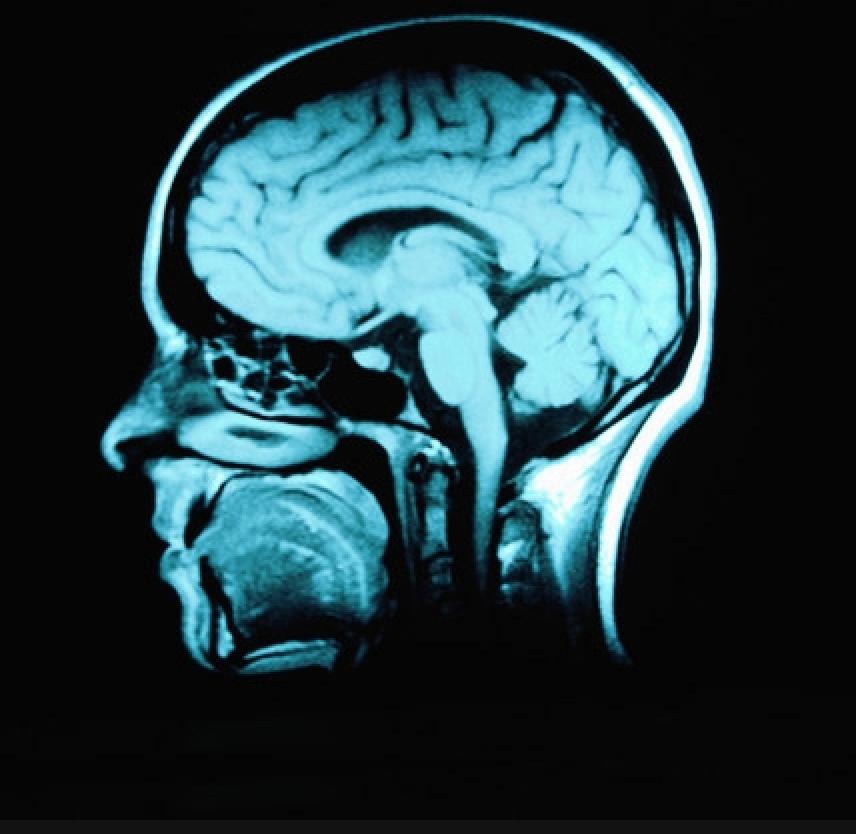
In closed head injury, damage occurs because the person receives a blow to the head that whips the head forward and back or from side to side (as in a car crash), causing the brain to collide at high velocity with the bony skull in which it is housed. This jarring bruises brain tissue and tears blood vessels, particularly where the inside surface of the skull is rough and uneven; damage occurs at (and sometimes opposite) the point of impact. Thus, specific areas of the brain - most often the frontal and temporal lobes - are damaged. This focal damage often can be detected through MRI and CAT scans.
In closed head injury, the rapid movement of the brain can also stretch and injure neuronal axons - the long threadlike arms of nerve cells in the brain that link cells to one another, that link various parts of the brain to each other and that link the brain to the rest of the body. This widespread axonal injury interrupts functional communication within and between various brain regions and sometimes between the brain and other body parts. However, this type of diffuse damage typically cannot be detected through currently available imaging technology (but with new developments, this may change). Its existence is very clear, however, in the widespread effects it has on the individual's functioning.
In sum, after a closed head injury, damage can occur both in specific brain areas (due to bruising and bleeding) and also be found throughout the brain (due to stretched or destroyed axons). The results of a closed head injury tend to affect broad areas of the individual's functioning, primarily due to the diffuse axonal injury. The extent of damage is correlated with the force of the blow to the head; for example, a head forced into a car windshield at high speed will tend to sustain more tissue damage than when the car is traveling at a slower speed.
Open head injury, the second type of TBI, occurs when the skull is penetrated, for example by a bullet. Damage following open head injuries tends to be focal, not diffuse, and the implications for subsequent impairment tend, also, to be focal and limited. However, such injuries can be as severe as closed head injuries, depending on the destructive path of the bullet or other invasive object within the brain.
What happens immediately after TBI?
Immediately following TBI, two types of effects are seen. First, brain tissue reacts to trauma and to tissue damage with a series of biochemical and other physiological responses. Substances that once were safely housed within the cells now flood the brain. These processes further damage and destroy brain cells, in what is called secondary cell death.
The second type of effect is seen in the individual's functioning. For those with more severe injuries, loss of consciousness (LOC) occurs at the time of trauma, lasting from a few minutes or hours to several weeks or even months. Lengthy LOC is referred to as coma. In such serious injuries, the first few days after trauma may also produce negative changes in respiration (breathing) and motor functions.
As an individual regains consciousness (those with the severest injuries may never do so), a variety of neurologically based symptoms may occur: irritability, aggression and other problems. Post-traumatic amnesia (PTA) is also typically experienced when an injured person regains consciousness. PTA refers to the period when the individual feels a sense of confusion and disorientation - Where am I? What happened? - and an inability to remember recent events.
As time passes, these responses typically subside, and the brain and other body systems again approach physiological stability. But, unlike tissues such as bone or muscle, the neurons in the brain do not mend themselves. New nerves do not grow in ways that lead to full recovery. Certain areas of the brain remain damaged, and the functions that were controlled by those areas may emerge as challenges in the individual's life.
Before discussing in greater detail what happens to the person after injury, which depends to great extent on the severity of injury, "severity" needs to be defined (in the next question).
What is meant by "severity of injury?"
Typically, "severity of injury" refers to the degree of brain tissue damage. Although the degree of such damage cannot be directly measured, it is estimated typically by measuring the duration of loss of consciousness (LOC) and the depth of coma (and sometimes by the length of PTA).
The scale most commonly used to measure the depth of coma is the Glasgow Coma Scale (GCS). The GCS is used to rate three aspects of functioning: eye opening, motor response, and verbal response. Individuals in deep coma score very low on all these aspects of functioning, while those less severely injured or recovering from coma score higher.
A GCS score of 3 indicates the deepest level of coma, describing a person who is totally unresponsive. A score of 9 or more indicates that the person is no longer in coma, but is not fully alert. The highest score (15) refers to a person who is fully conscious.
Severity of injury is typically categorized into three levels: mild (or minor), moderate and severe. A commonly used rule of thumb is that mild injury refers to LOC of less than 20 minutes and an initial GCS of 13-15. Typically, an initial GCS of 9-12 defines a moderate injury and 3-8 a severe injury.
Although initial "severity" measures may generally predict long-term impairment, initial severity scores do not correlate well with negative consequences in a person's life. The effects of TBI on individuals and the meaning of those effects depend upon a wide variety of factors, only one of which is initial "severity of injury."
How long does recovery take?
Recovery after injury is usually quite different for those with moderate-to-severe injuries versus those with mild injuries. And, as must be constantly kept in mind, recovery varies greatly from person to person. Thus, recovery will not be the same for any two people with TBI.
In mild TBI, one person may recover quickly and completely, while another may experience significant challenges even several years after injury. (Recovery after mild TBI is discussed more fully in a later question, What Impact Will Mild TBI Have ona Person's Life?)
In more severe injuries, recovery is a multistage process, which typically continues in a variety of ways for months and years. However, the length of this recovery process is not uniform, and the stages of recovery that are typical when considering the population as a whole, may be very different for any specific individual. Stages may not proceed step-wise but may overlap, one stage with the next, or one or more stages may be skipped altogether. The early recovery process is discussed more fully in the next question.
How is recovery measured right after injury?
The progress seen during the immediate recovery period in individuals with severe to moderate TBI is often tracked using the Rancho Los Amigos Scale, which specifies eight levels - from the depths of coma to return to awareness and purposeful activity. These levels of recovery of functioning reflect processes within the brain, as it heals, stabilizes, and reorganizes itself to some extent.
Although the Rancho scale assumes that recovery will pass through eight stages, a small percentage of people with severe injuries remain stuck at Levels I to III for months or years. They remain in coma or in a relatively unresponsive state and fail to return to purposeful, appropriate functioning.
Rancho Los Amigos Scale
- Level I (No Response): The individual is in deep coma and does not respond to any stimuli.
- Level II (Generalized Response): The person sleeps most of the time, with periods of brief wakefulness. Responses and movements are largely reflexes not purposeful.
- Level III (Localized Response): The person is alert for lengthier periods. He/she reacts inconsistently to commands, but his/her responses are related to the type of stimulus presented. For example, noises will produce a listening response.
- Level IV (Confused and Agitated): As awareness increases, the individual's behavior reflects his/her sense of confusion and disorganization. Aggressive and/or silly behavior may be seen, with verbal abuse, agitated actions, and incoherent speech. The person's attention span is too short to allow full cooperation in treatment programs; and the person is unable to do basic tasks, such as eating, independently.
- Level V (Confused, Inappropriate, Not Agitated): Simple commands are now followed consistently; the person's long-term memory is returning; and she/he can now carry out over-learned skills such as eating. Difficulty is evident in following complex commands, short-term memory, learning new skills, and concentrating for more than a few minutes.
- Level VI (Confused, Appropriate): The individual begins to show goal-directed behavior, but usually still needs direction. The person is more aware of his/her deficits, family members, and so forth. He/she can carry out more tasks independently and retains relearned skills from one occasion to the next.
- Level VII (Automatic, Appropriate): The individual performs daily routines automatically and is better able to learn new skills, although slower than before injury. The person still has poor short-term memory; judgment and problem solving are still impaired.
- Level VIII (Purposeful, Appropriate): The person is able to function once more in the community. Impairments in cognitive, social, and emotional functioning, to a greater or lesser extent, may continue.
FromIcahn School of Medicine at Mount Sinai. icahn.mssm.edu

Comments (131)
Please remember, we are not able to give medical or legal advice. If you have medical concerns, please consult your doctor. All posted comments are the views and opinions of the poster only.
Anonymous replied on Permalink
I believe I have a very unique traumatic brain injury.
I contracted leptospirosis while grooming a dog which temporarily shut down my immune system which then caused a staph infection in my right kidney. My doctor put me on malaria inhibitors, strong antibiotics and steroids to try to stop the staph & lepto from causing renal failure and apparently the leptospira went into my brain and nervous system trying to hide from the antibiotics that were being distributed through my bloodstream. So I had a leptospirosis brain infection while my immune system was effectively turned off by the leptospirosis
which then damaged the nerve cluster in my brain and made it short circuit which gave me SEVERE right trigeminal neuralgia then right occipital neuralgia then bilateral carpal tunnel and right arm pain and weakness and now I have spinal stenosis causing severe nerve pain down my left leg.
I didn't even know I had a traumatic brain injury until 8 months later when my doctor noticed I could barely write and I mentioned it made my hand hurt and I hated that my handwriting was completely different before my head short curcuited because it went from cute and girly to completely different manly scratches and the doctor then informed me that that was a sign of me having a traumatic brain injury.
Which suddenly made sense with all the forgetfulness and confusion and and messed up equilibrium issues I was having.
My TBI happened in 2007. I still can't remember 2006.
Crystal LEDBETTER replied on Permalink
Thank you for the article it offered the best explanations i have read so far and i am actually a medical professional with over 20 years experience. i found this to be easy to read and understand and extremely informatable. I was searching for information because a friend had hit his head and refused to go to the ER, however after reading this i am making an appointment for myself to have a CT scan. 2 years ago i was in an abusive marriage and I suffered 6 head injuries i had thought to be minor at the time. due to the nature of the injuries i never sought treatment for them and now i currently suffer from constant blurry and decreased vision, at times i have a headache so severe it causes nausea and vomiting about 3 times a month, and once i vomit it seems to subside. i also have short term memory loss and actually have trouble with things i use to do with my eyes closed. I have difficulty at times preparing a meal and to be honest i never realised i may have brain damage from all the trauma so i greatly appreciate the article
Pamala37 replied on Permalink
My third child, Rebekah Abigail was killed instantly at age 27. She was in a fatal car accident that the prongs of a corn plow went through her windshield into her fronal lobe. Our daughter did not suffer, a blessing that she was taken so quickly. Because she was an organ donor she was kept on life support until they could harvest her organs, saving other lives. I have peace knowing we will see each other in Heaven one day. Becky had two older sisters, one younger sister and brother. She was gifted to us from God for 27 amazing years! Her cause of death was TBI. Sadly, her siblings still grieve over her passing. Interestingly, Rebekah had called me 2-3 weeks prior to her accident, telling me that "God is taking me home early...I wish to be buried in a pine box, no funeral, simply a celebration of life service". When I got that call in the middle of the night, I knew it was about Rebekah. Although she tried to warn me, I fell to my knees, ripping my nightgown in half, wailing until my husband and son heard me.
To this day I see Gerber Dasies everywhere (Becky's favorite flower), sometimes I even smell her or feel her presence frequently, which comforts me greatly!
Lana replied on Permalink
Wow, Becky knew. That’s amazing. Peace be with you my friends.
Katrina replied on Permalink
I researched this article, as a family member is currently in a coma after a RTA on sunday, and still not awakened, and I came across Rebekahs story and I was struck by the line " Rebekah had called me 2-3 weeks prior to her accident, telling me that "God is taking me home early...I wish to be buried in a pine box, no funeral, simply a celebration of life service". When I got that call in the middle of the night, I knew it was about Rebekah."
God had prepared Rebekah that she was going to be leaving this world and entering her eternal body...that really is incredible.
I lost one of my teenaged best friends last year- she died from cancer 6 weeks after she found out she had it, and her father spoke at her funeral about her being the first born, and the first night when they brought her home and put her down to sleep, her father said he sat there and watched her sleep and marvelled at how incredible she was, and thanked God for gifting them this precious child, and he said he clearly heard an audible voice say to him "I am preparing you with the knowledge that you will have this child for a time, but not a whole life time" and he was shocked by what he had experienced and tried to put it to the back of his mind, but his beautiful daughter did leave this world when she was only 49 and way too soon, but she loved the Lord and sang of the Goodness of God until she no longer could sing, a week before she passed.
I also know of a little girl, also called Rebekah, who was 8 yrs old when she got out of bed one night and came downstairs and told her parents "I'm going home!".
Her parents tried to shush her and send her back upstairs, but she again said "God told me I am going home soon!".
They thought she was being silly and sent her off to bed, but the next evening, she had a massive Asthma attack and couldnt be saved.
Her mother said looking back at that incident, there was no fear or sorrow in her daughters voice, she announced it as if she was excited about it, but they thought nothing of it as they just thought she was being silly and half asleep.
We are all just passing through this life, and my experiences have taught me, that through it all, he holds us in his hands.
Kira replied on Permalink
My mother was the pedestrian victim of a hit and run in October of 2016. She spent a few months in a coma. She had started to open her eyes and move slightly in December. On Christmas she spoke for the first time since the accident. It has been a long, slow road of recovery, and she may always be paralyzed on the right side of her body. Her cognitive function has slowly returned though. Over the last 5 years, I have watched as she slowly got better. Is it possible for someone with a severe brain injury to reach level 7 or 8 on the rancho los amigos scale so long after the initial event? I feel like she is now at a 6, but I hope for more one day.
Matt replied on Permalink
My brother was on a bike and hit by a car and he was in ICU for 3-4 days. During the time, the doctor opened up his skull and cut off and removed a few parts of his damaged brain due to blood pressure and etc. Since the operation, my brother is still in a coma after 14 days.
The doctor had a scan for his brain 2 days ago and told us that he will never be fully recovered and the best outcome will be he is in a wheelchair and be able to eat.
My questions are:
- why did the doctor cut off and remove a few parts of the brain due to blood pressure instead of extracting the blood from his brain?
- will my brother has a better outcome than can only be able to eat in a wheelchair and not even knowing who he is?
Thanks, everyone.
Miles replied on Permalink
Closed Head Injury is similar to a concussion that you can recover. because i forget to wear the helmet on my bike riding.
Anonymous replied on Permalink
my mom was in a motorbike accident. They hit the rail of a bridge and she flew 30 Meters down into a river bed landing on a rock. Her helmet was not even scratched. She was declared Dead on Arrival. The said blunt force trauma to the head. I went to identify her body and did not see any open wounds. What keep me up at night, she must have known flying in the air what was going to happen. If she injured her head on impact, would her brain still have been active
Anonymous replied on Permalink
I hope I can give you some peace with your question. I was a police officer for over 10 years and worked many fatalities from vehicle accidents during that time. I was very bothered by those at the time and, for some reason, even more bothered by them after leaving law enforcement. I just couldn’t forget the violent manner in which these people seemed to die in such a random manner and it bothered me.
Now, fast forward over a decade and I was recently involved in a MVA that easily could have taken my life and the life of a passenger. We were hit by a drugged driver, cut from the vehicle by the rescue crew, and were both transported to 2 different hospitals. My passenger by helicopter and me by ambulance. My brain was bleeding in 2 different places and I was unconscious.
I remember nothing about the accident. My first memory was waking up in a CT Scan at one of the hospitals and I must have passed out again because my next memory was waking up in a recovery room at the second hospital. I don’t recall the feeling of pain though my wife tells me it was obvious to others. I was also conscious at times and saying things to healthcare workers that I don’t recall.
Months later, I am still having difficulty with so many things and my memory of things since the accident is terrible. I can write and do math apparently about as good as I ever did. I struggle with reading some, but I doubt it is noticeable to other people.
One thing that has brought me some peace as a result of the accident is that I no longer worry about those people who lost their lives in the crashes that I worked. If I had died that day, it would have been a peaceful experience. I know that is hard to understand by the people who saw me suffering after such a violent collision, but it is true.
I hope you will find some peace in the fact that people who meet traumatic experiences as you describe with your mom are protected by their brains in ways that people who have not lived through such an experience cannot understand, but it is true. I am not just saying this to be nice either. I really do believe and understand this now. I hope you can trust that your mom did not suffer needlessly. We are wonderfully made and our brains are not easily understood. I can say that even with the problems I am experiencing now.
Anonymous replied on Permalink
Thanks for sharing that perspective.
Anonymous replied on Permalink
my niece had a massive heart attack her heart stop beating and there was brain damage ,now the doctor said her brain is sliding what does that mean
Anonymous replied on Permalink
Hi, my brother is being shot on his head 3x so now for a week his been in ICU and we don't even allowed to see him because he is still under police supervision all I want to know is he going to make it out of ICU and gain memory in time? They said he needed more blood and got it on the 28th January 2021 after he was shot on the 26th January 2021.
Anonymous replied on Permalink
It is possible but not always that the person makes it so you're relative has a 50/50% chance. At the speed that he got blood he should be okay though. So don't worry
Anonymous replied on Permalink
My Cousin 18-year-old male In perfect health. Got stabbed, two knives to the heart which caused heart damage and also lack of oxygen to the brain. Doctors believe that he liked oxygen to the brain for 45 minutes prior to ambulance arrival. After his heart Mc surgery he is now in a coma. and we don’t know how much brain damage there he is no responding to any test that Dr's are doing. Is there any chance he will ever recover from it. I would like a professional opinion if there’s hope for this young kid who’s fighting for his life.
Unknown replied on Permalink
Yes there is a chance depending on how bad it is.
Anonymous replied on Permalink
how is he?
Anonymous replied on Permalink
I think alot depends on if his brain was recieving oxygen during those 45 minutes and how much. After 3 to 4 minutes with limited oxygen to the brain permanent brain damage can occur. Best wishes. JAnderson Lpn
Soren replied on Permalink
I was on my knees slowly going toward my dog, and my sister pushed me not too hard but medium. I hit the side/ front of my head on our pool table's edge. Nothing really happened at all but I got a headache and now about 14 hours later have a migraine. It feels like a thumping heartbeat in my head, and it is annoying. I got sleepy after like 6 hours from the hit, and yeah I don't know. My mom and everyone else says I will be fine, but I just can't fall asleep. I am too scared to have permanent damage since I am a very smart person who just wants to live my life happily.
Anonymous replied on Permalink
Sorry, my mistake. I was in a coma for a month, icu for another month, and in inpatient rehab for another month. Took me a while to get the ok to just leave the yard. I was always a city person, but now I am a small country person. Village only has about 700 people. I can walk again, talk again, even shop again. God is good and now I am just waiting for the next thing I am going to be given. Just say a prayer for me and make me "up for the challenge".
Rose Gordon how replied on Permalink
How long it took u to woke up cause my boyfriend hit is head for four weeks now and he is still in coma a sleep
Meaghan replied on Permalink
I just read your comment and I thought it was brave. I just came home from 6mths in hospital after I had a car crash. Apparently I dont drive too well ! I have a brain injury and I can relate to everything you said. I said a prayer for you, I hope it helps you. Please feel better and never lose your brilliant attitude. Thanks for reading. Bye now.
Annon replied on Permalink
Hi there my brother in-law was in a car accident he's currently got heaps of small holes in his brain and they say it's not looking like he will recover can u send some light towards your brain injury
Lisa replied on Permalink
My son was in motocross accident he has surgery on the brain . For aneurism he had shunt put in few days ago he has eyes open he does move eyes back forth little looking at nurse I think he’s been icu four weeks this surgery just three days they said we need find long term care place for my son he’s young and a fighter what is the best Ext step for him I don’t want him laying in bed in a place where old people go I want them work which him so he can respond and get better he’s a fighter San diego
Anonymous replied on Permalink
Well listen to what they are saying. And find the best place for your son.
Brent replied on Permalink
Hi. I am 43 years old and 2 1/2 years ago I was hit by a Hummer. He had a red light and I was in the crosswalk. I had 10 rib fractures, one went and burst my lung, my esophagus burst, and I had two broken head wounds. I was sent into critical care surgery. During surgery they took off half of my skull to alleviate pressure and during surgery I had a stroke and died for 2 a half minutes and those are the 2 and a half minutes I do remember. I made it through surgery
Vishwa replied on Permalink
Today when I am eagerly waiting for my father law who is in ICU undergoing brain surgery, I realize how much painful it would have been for you to pass that time in operation theater, those two minutes, entire life would have flashed through and gone like cool breez, feeling numbness. I pray to God to keep you healthy
John J Brown replied on Permalink
I was in a car accident in June 2019, I was hit from behind at over 60 miles an hour I was at a red light, my head hit the strearing wheel, I los conciousness now my speach is slur, I drool from my right side, I dont breath normal, I forget wear I'm at, I dont feel my hands I dont feel when I'm hungry.i forget information, I can only sleep1 to 2hrs at a time. This is happening even after 7 month .
IT dont seem like all these symptoms are going to change. Am I going to be scared for life with these symptoms
Anne replied on Permalink
Keep praying! God can do all things! I was riding my bike on a highway and got hit by a truck going 55 miles an hour when I was 14. In a coma a week or so. I dont remember anything. Had to relearn to read do math etc. But time and God healed me. Still have difficult times 25 years later mentally and emotionally but God is good. Sending prayers to you and everyone here who needs them!
Anonymous replied on Permalink
How right you are! Life and death is in God's Hands alone. Sometimes He choses to heal us, other times, take us. God doesn't ALWAYS answer in the way we want or expect, through prayer He will give us both peace and understanding! I have yet to have any prayer go unanswered.
Kevin Huff replied on Permalink
I'm sorry that you are having issues. Its been 30 years since my coma and I'm still having issues. However, it took me a year and a half before I started to feel almost healed. Still have brain issues, speech, thought, walking, emotional and attachment issues with relationships. Be patient. It takes a long time to heal. I was only in a three day coma after a bad ski race fall. I will be dealing with issues the rest of my life but, I will not give up!! Never! God Bless and hang in there!
Anonymous replied on Permalink
I suffered from two gunshot wounds to the inside of her head on the right side how long will it take for my recovery process and I have a bullet still lodged in my brain
Anonymous replied on Permalink
My father is 58 years old he was in an Bike accident it has been 18 days and he is still in coma I m so stressed reading all day about the injury he sometimes opens his one eye moves his legs and hands My family is so tensed I wish this won't happen to anybody It's been a hell of trauma to my whole Family I cry every night thinking what could have happened how he could have been saved from the injury
God help us
Anonymous replied on Permalink
How about your father now?
Tushar shety replied on Permalink
My father also had the same case as your but he is only 51 years old and it's 19 days he is in coma ...me and my family are fully depressed ...
Anonymous replied on Permalink
Hi several months ago my wife age 76 yrs was killed instantly in a head on car crash i was with her in a min or less she has a lot of body damage to her arms legs an a broken neck but no blood was flowing from any of her wounds why the only blood was from her nose an left ear an it only covered the palm of my hand , need some idea of what caused no other blood loss from any of her sever wounds Thanx
Kelli replied on Permalink
I don't know.. I was a pedestrian, hit by a car going 50mph. I had over 40 broken and fractured bones. Colapsed lung and hematoma in frontal lobe. I implanted in the windsheild, denting the roof of the car about 8" back. Months later, came across the clothes I was hit in. And that was my first thought.. I only had one inch or two round spot of blood. Oh and they didn't cut my clothes off me. But it was weird. Like my body just broke.
Anonymous replied on Permalink
Did they tell you that she may have had internal bleeding?
Amanda replied on Permalink
My dad was only 50 years old newly sober from alcohol and I mean very new. He fell at home and hit his head and ended up bleeding out over a period of numerous hours without calling for help. When his mother found him two days later they had to call the polic my dad was only 50 years old newly sober from alcohol and I mean very new. He fell at home and hit his head and ended up bleeding out over a period of numerous hours without calling for help. When his mother found him two days later they had to Call out homicide detectives because of the amount of blood all over his house they thought somebody had murdered him. The detective reassured me six months later after the final autopsy that it was an accident that he just hit his head and was too confused to call for help how is this possible how do you not call for help
Anonymous replied on Permalink
Am cecilia.am a care worker I am looking a traumatic brain injury patient he was in car eccident 2015 he can't talk can't even walk see he can't but now his suffering from headech scratching his head he can't sleep he during the day after session he need more support
Dianne replied on Permalink
Hi Amanda, your story resonated with mine. My 63 year old sister fell at home, I found her and think it may have happened between 10 and 20 hours before being found. There was blood everywhere and her death was with the coroner until it was determined that she went into cardiac arrest. I don't know if that happened before or after the fall. What a distressing thing for your grandmother to see, she will never recover from that.
Saly replied on Permalink
I'm really sorry to hear about your dad.
Courtney replied on Permalink
Mm, i dont think i had it that bad.. i flew off a snow tube, went up in the air, landed exactly upside down. I couldnt eat for a long time. I had spasms. Couldnt move. I couldnt understand 90% of what people were saying to me for 6 years. Anything that wasnt a direction I could not understand. I could work i just couldnt understand simply what "hello" meant. I didnt say anything. Couldnt remember who people were. I just remember throwing my shoulders backwards as possible and making my shoulders an attempted shield to my fall by jacking them up to get the brunt of it. I slid down the snow tube hill backwards, body up, on my neck and back of my head.. numb. Couldnt feel my tongue. I laughed when I was rescued. I remember all the inabilities I had and everyone bullying me. I got traumatised to no end. I could only do commands.. i barely could survive but I did. I had to act crazy to get people i didnt wanr near me away from me because I was so dumb that I didnt know my ABC's.. it sort of worked. Just overkill. Better than people getting closer to me and being vulnerable right. Everyone bullied me and accused me of doing heroin. That shit is nasty. Its funny because i hate drugs. Then i was accused of being a prostitute. I was stalked, bullied. All during a time i barely understood anything. I got stabbed in the back. It just goes on and on forever. I knew acting sort of. That was cool. I think I recovered after 7 years and was able to fully function again. Ptsd though, was not fun. Being abused for being stupid wasnt fun. It was being snuffed, and I didnt like it what so ever. 99% of people will kick a person with a spinal injury down and that is the truth, at least for this area.
Brietta Walker replied on Permalink
April 25th 2019 my husband was in a horrible car crash. I know it's too early to tell but in all honesty I am scared senseless. This is the first time this has ever happened to me, and although he is doing pretty good (I think) when he did look at me, he gave me a weird look like he didn't know who I was. Is this normal? Will he ever actually remember who I am or what I am to him?
Emily replied on Permalink
My partner was also in a terrible crash and has a hard time recognizing people, including me. How is your husband now? Did his confusion resolve?
Jake replied on Permalink
I was in a car accident April 19 2019.
I was diagnosed with multiple neck, back and abdominal injuries. As well as a closed head injury with LOC and a separate head injury. Since then, I’ve been stuttering a lot, and I’ve been having a hard time keeping a conversation. I had so many conversations end awkwardly on Easter. Swallowing has been difficult. I forget things so quickly. I’m worried about this. I don’t have health insurance but the accident was the other drivers negligence. I ran head on into her driver side door. Air bag saved my life. I just don’t feel like myself right now.
Kim replied on Permalink
July 16, 1996, I‘ve been told I was in a car wreck. I’ve been told I was in a coma. What I call my alive day, July 24, 1996, is the day I came out of the coma. I cracked the left side of my skull on the A post of my Wrangler. I broke both bones in my lower left arm. I was told it’s due to me trying to shield my head from the impact. My left leg was broken in 5 places, 2 of those were in the neck of the femur which could have been possible to cause my bone to die and resulting in my loosing my left leg. Thankfully that didn’t happen. I fractured my left hip. The muscle at the base of the femur degloved (that’s where there’s a severe and direct impact of great force, causing the muscle to be torn away from the skin and pushed aside.) That muscle is still displaced; it resides in the back of my leg rather than on the side. The doctors didn’t replace it because they didn’t believe I would recover. After waking from the coma, I had multiple nurses and doctors tell me I had a severe head trauma but nothing was ever said beyond that. I’ve only in the last 5-6 years learned that some of the issues I’ve had since then are related to the TBI. The insomnia that gets me every night is related to the TBI. The fact that I am an agoraphobic is another result. Crowded places, whether it be people or stuff makes me feel like I’m trapped and can’t move; can’t breathe. Going to new places is a huge issue for me. I have to do things in specific orders. If my routine is out of order, I will forget something. Such as in the morning when getting ready for work, if I put my hair up in a pony tail first, I’ll forget to brush my teeth and put on deodorant. If I put deodorant on first. I’ll forget to brush my teeth. If I don’t hang my keys up as soon as I walk in the door at home. I won’t remember where I’ve put them. I have issues when it comes to remembering numbers now. I have times when I’ll be asked a question, I’ll answer the question and not realize that I didn’t verbalize the answer. I apparently will think the answer in my head and fail to say the answer. That doesn’t happen very often. Often times, I can’t remember what something is called. Such as one night I was trying to describe the nice cool breeze coming through the skylight. I couldn’t remember skylight so I said “that hole in the ceiling with the cover over it”. I’ve forgotten my son’s name only twice in his life. I have a hard time remembering how old I am. I guess it’s the number thing. I’ve noticed that when I am very tired, I tend to stutter more than I usually do. If I’m stressed out, my insomnia worsens and I tend to forget words more often.
As much as I can’t remember things, I used to work at a county jail, passing medications. I had over 300 inmates to pass meds to and I could highlight their names on the rosters without going by the MAR to highlight their names. When they approached my med cart, I knew their names. I even knew what medication they received as well as the dosage. I could also remember their allergies which helped out a few times. I would point out to the doctors their about a script they’ve written to an inmate that they were allergic to.
In fact, all the locations in which I worked as a nurse, I could remember all my patients (and inmates), their medications and their allergies. I could also give you the brand name as well as generic names to all medications and I could list all their uses and adverse reactions, whether it be from the medical side or the mental health side.
I can tell you that none of my “symptoms” have worsen. I can’t say that they’ve improved. I can see a difference when I do those brain game puzzles.
When I worked at the jail, I met an officer that received a TBI a year after I received mine. He’s the one that taught me about my tbi. He’s the one that helped me realize that all those listed above were directly linked to the tbi. He helped me not feel so stupid when it came to those listed above.
There’s only two things that some people in my life have said to me that causes me to immediately get angry with them. That’s when they say it imply that I’m faking my symptoms. Also when they say “I know you don’t understand this....”. Although I do get angry with them for saying those to me, my anger never stays. I’m only angry for a few minutes.
When I first woke up from the coma, I didn’t know about anything past the elevators. I didn’t know outside. I didn’t know I had a home. I had to be reminded who my mother was when she first came to visit me. I basically started my life on the 24th of July in 1996 but whenever I heard a song, whether on the tv or the radio. I knew all the words to that song.
Donna replied on Permalink
TBI is a terrible thing. I am so sorry you've had to go through what you've gone through, Kim! I sure hope things are improving for you! My ex father-in-law only improved due to being treated in a rehab facility that specialized in tbi. I don't know if you have one around you, but it may be worth looking into?
Brad Lancaster replied on Permalink
I was hit by a tree I was cutting down and was in a hurry but obviously didn’t plan it very well
Because I forgot to buy a new blade for my chain saw but kept going anyway thankfully my niece and her husband were with me
When I was finally out of my medically induced coma I was very agitated almost pissed off
I didn’t understand what had happened but because of my brain injury I was kept in the hospital for I think two months
They wouldn’t release me I couldn’t swallow and was having trouble breathing so I was put into a va rehab center until I could perform certain daily functions like swallowing walking up and down stairs with and eventually with out a cane because my leg was broken by the impact of the tree Later I was told that when the tree hit me it drove me down like a hammer hitting a nail all that I can remember is feeling confused and falling back on my ass and tried to pick up my leg and realized it was broken and then I passed out lucky for me my nieces husband realized what had happened to me when saw me bleeding for my ears nose and eyes and yelled to my niece to call an ambulance when the ambulance arrived I was lucky again the medic that came realized I was bleeding badly from my and cut me below both eyes to relieve the blood pressure on my brain because of the severity of my brain injury they determined I wouldn’t live long enough for them to drive me an hour away to Cleveland university hospital they called for a life flight and were able to land in a nearby field and fly me to Cleveland
That was I think ??????? In 2017 but still not sure and here I-am in 2022 and I’m still having problems remembering what should be simple thing like writing thankfully for technology or you wouldn’t be able to read this I still can’t remember how to use my cell phone But I’m still trying and everyday is still tuff as hell I have copd because of smoking since I was 21 in basic training at Lackland AFB in San Antonio Texas and I-am 65 today but I still know that day in basic was my 21st birthday was when I started smoking we were standing at attention and our drill Sgt said okay men at ease and smoke them if you’ve got them so I asked another trainee if I could borrow a smoke and he said how are you going to pay me back if you don’t even smoke so I said I promise you I’ll pay you back so we were trained to always be a man of your word and to never let another soldier down I bought a pack the next day and gave him back his smoke and you all know smokes aren’t cheap so I paid for them with the very little money I had left and continued to smoke even if I was out because now I could bum a smoke from almost anybody one day when our instructor said smoke them if you’ve got them I didn’t have any but everybody that smoked was out and I said excuse me sir but can I please borrow a smoke and he said you know what to do So I marched up and did a left face so I was in front of him and saluted him even though he was a Sargent technically I wouldn’t have to salute him but we were taught when addressing him we must treat him as a superior officer and said sir yes sir may I please have a cigarette while still holding myself at attention and still saluting he took his pack out and held one out to me I said thank you sir and he said at ease airman then I was able to drop my salute and accept the cigarette I put the smoke in my front but hadn’t remembered I didn’t have a lighter and had to stand at attention and say excuse me sir while standing at attention and saluting again may I please borrow your lighter he said at ease airman and handed me his lighter and I said can I please hang on to it till after we’re done with our drills and he saluted me back and said permission granted so I marched back into formation and staid at attention and he yelled lancaster and I yelled back sir and he yelled at ease and I yelled back thank you sir and lit up my smoke So any of you that have been in the military know that is how it is when your in the military also that practice will make you a perfect soldier
So the best thing I can tel you all with tbi’s Practice Practice Practice practice I still to this day believe I have psychotic delusions and am still trying to get back to rehab because of memory issues So to all of you out there with memory issues hang in there and surround yourself with people that care about you and if there are people in your life that don’t care Think about it for a very long time and after you’ve decided not because I said so
Walk away that’s some of my best advise to you all Only you can decide for yourself but be very careful that you decide for yourself Good luck !!!!!!!
Karen E replied on Permalink
My brother in law has a brain injury from a car accident. It's been a couple of years now and where his scar is it looks like it's sinking. What could this be?
Pages